When you pick up a prescription, do you ever check if it’s the brand name or the generic? For most people, it doesn’t matter-until it does. Suddenly, the pill looks different. The size is off. Maybe it tastes weird. And then, without anyone saying it out loud, doubt creeps in: Is this really the same?
This isn’t just about packaging or price. It’s about trust. And trust, in medicine, is everything. Even though generics are chemically identical to brand-name drugs, patients often feel like they’re getting the second-best option. That feeling? It’s not irrational. It’s psychological. And it’s measurable.
Across the globe, millions of people take generic medications every day. In the U.S., 90.7% of prescriptions filled are generics. But only 22.8% of total drug spending goes to them. That’s because generics cost a fraction of the brand name-sometimes 90% less. So why do so many patients still hesitate? Why do some swear their generic statin doesn’t work like the brand? Why do others report side effects they never had before switching?
The answer isn’t in the chemistry. It’s in the mind.
What Patients Actually Feel About Generics
Studies show that patient satisfaction with generics isn’t about whether the drug works-it’s about whether they believe it works. A 2024 study in Nature Communications found that 72% of patients reported dissatisfaction with at least one generic medication they’d taken. The biggest reasons? Perceived ineffectiveness and negative perceptions about quality.
One patient in a Reddit thread wrote: “Switched from brand-name Synthroid to generic levothyroxine and my TSH levels became erratic.” Another said: “Generic lisinopril works exactly the same as Prinivil but costs $4 instead of $40.” Both are true. One is a medical fact. The other is a lived experience. And in healthcare, lived experience often trumps data.
It’s not just anecdotal. Research using the Generic Drug Satisfaction Questionnaire (GDSQ)-a validated tool with 12 items-shows that effectiveness, convenience, and side effects account for 66.8% of overall satisfaction. But here’s the twist: effectiveness ratings are heavily influenced by expectations. If a patient believes a generic is inferior, their brain is more likely to interpret normal fluctuations as side effects or failure.
The Psychology Behind the Perception Gap
Brand-name drugs come with decades of marketing, glossy packaging, and doctor endorsements. Generics? They come in plain white pills with a manufacturer’s code. No story. No history. No emotional weight.
This is classic brand psychology. We associate price with quality. We associate familiarity with safety. We associate name recognition with reliability. Even when the science says otherwise, the mind defaults to what feels familiar.
Studies in cross-cultural psychology show this effect is even stronger in individualist societies like the U.S. and Australia, where personal control and choice are highly valued. In collectivist cultures, patients are more likely to trust authority figures-doctors, pharmacists-over their own assumptions. That’s why satisfaction scores are 32% higher in countries like Japan and Saudi Arabia, where physician recommendations carry more weight.
And then there’s the placebo effect-but reversed. It’s called the “nocebo” effect. When you expect a drug to cause side effects, your body is more likely to produce them. One study found that patients told their generic medication might cause headaches reported them 40% more often than those told the same pill was “identical to the brand.”
How Satisfaction Is Measured-And Why It Matters
Satisfaction isn’t just a feeling. It’s a metric. And it’s tied directly to whether people take their meds.
Non-adherence to medication costs the U.S. healthcare system $300 billion a year. A big chunk of that? Patients stopping their generics because they think they’re not working. That’s not just a financial problem-it’s a health crisis.
Researchers use several tools to measure satisfaction:
- Generic Drug Satisfaction Questionnaire (GDSQ): A 12-item survey measuring effectiveness, convenience, and side effects. Reliability scores (Cronbach’s alpha) range from 0.78 to 0.89-solid for patient-reported data.
- Discrete Choice Experiments (DCE): Patients choose between hypothetical drug profiles. This reveals what they truly value-price, pill size, frequency, side effect risk-even if they can’t articulate it.
- Machine Learning Models: A 2024 study in Greece used a Random Forest algorithm to predict generic acceptance with 89.7% accuracy by analyzing 15 variables: age, income, education, prior experience, provider communication, and more.
Here’s the catch: the tool you use changes the answer. DCEs show latent preferences-what patients would choose if forced to decide. Surveys show stated preferences-what they say they believe. And they often don’t match. One study found that 69.8% of patients said they’d accept generics if their doctor recommended them-but only 45% actually did when given the option without explanation.
What Works: How Doctors and Pharmacists Can Make a Difference
Patients don’t trust generics because they’re bad. They distrust them because no one told them they’re good.
Research from the University of Amsterdam and Harvard Medical School agrees: generics are just as safe and effective as brand-name drugs. But that fact only matters if it’s communicated clearly.
Here’s what works:
- Explain bioequivalence: Tell patients the FDA requires generics to be within 80-125% of the brand’s absorption rate. That’s not a loophole-it’s a scientifically validated range.
- Normalize switching: Say, “Many patients switch to generics without issue. I’ve seen it work for hundreds of people.”
- Address fears directly: If a patient says, “I had a bad reaction,” ask: “Was it the pill, or how you felt about the pill?”
- Use visuals: Show side-by-side images of brand and generic pills. Point out the identical active ingredient listed on the label.
A 2023 study in Saudi Arabia found that when physicians explained FDA standards, patient satisfaction jumped by 34.2%. That’s not magic. That’s communication.
Which Medications Cause the Most Problems?
Not all generics are created equal in the eyes of patients. Satisfaction varies wildly by drug class:
- Antibiotics: 85.3% satisfaction. Easy to judge-fever goes down, cough clears. No mystery.
- Statins: 71.2% satisfaction. Some patients report muscle pain or fatigue they didn’t have on the brand. Often, it’s psychological.
- Antiepileptics: Only 68.9% satisfaction. This is the big one. Even a small change in blood levels can trigger seizures. Patients are terrified. And rightly so-this isn’t just perception. There’s real clinical risk if switching isn’t managed carefully.
- Antidepressants: 65.1% satisfaction. Reddit threads are full of stories about mood swings after switching. Some are real. Some are nocebo. But either way, they’re real to the patient.
For drugs with a narrow therapeutic index-where the difference between effective and toxic is small-doctors should proceed with caution. But for most others? The data is clear: switching is safe.
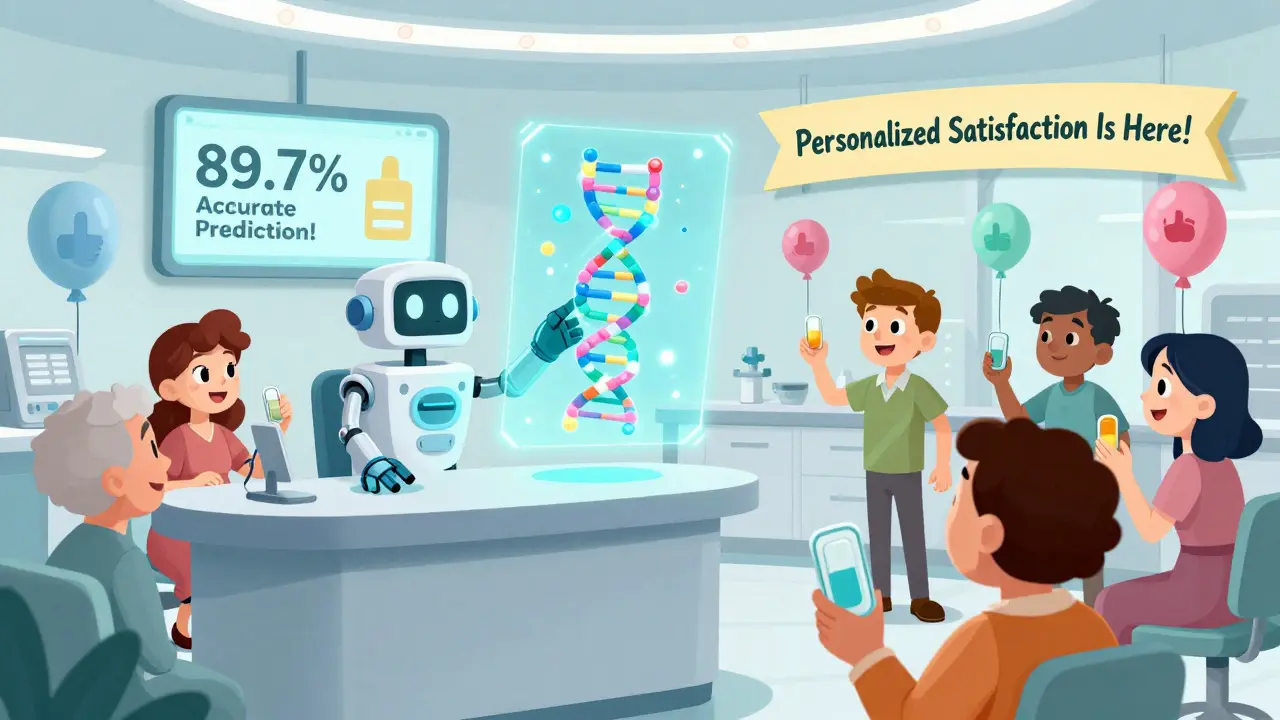
The Future: Personalized Satisfaction
The next frontier isn’t just measuring satisfaction-it’s predicting it.
The Mayo Clinic is piloting pharmacogenomic assessments that look at a patient’s DNA to predict how they’ll respond to certain drugs. Early results show a 28.7% improvement in predicting satisfaction compared to traditional surveys. Imagine knowing before you even prescribe: “Based on your genes, you’re more likely to react negatively to this generic form of sertraline.”
The FDA’s new GDUFA III initiative is investing $15.7 million to build smarter tools. The European Commission is scanning half a million social media posts in 28 languages to map how people talk about generics online. Sentiment analysis is revealing that patients who mention “cost savings” are 3x more likely to stay on generics-even if they complain about side effects.
Generics aren’t going away. They’re essential. But for them to work-not just as drugs, but as solutions-we need to fix the story around them.
What Patients Can Do
If you’re on a generic:
- Don’t assume a change in how you feel means the drug isn’t working. Ask your pharmacist: “Could this be a change in fillers or coating?”
- Keep a simple journal: Note when you take the pill, how you feel, and any symptoms. Patterns matter more than single bad days.
- Ask your doctor: “Is there a reason I’m on this generic? Is it safe for me?”
- If you’re unhappy, don’t stop. Talk. There’s often a different generic brand available that might work better for you.
And if you’re a provider? Don’t assume patients understand what generics are. Don’t assume they’re grateful for the cost savings. Ask them. Listen. Then explain-not with jargon, but with honesty.
Generics save lives. But they only work if people take them. And people only take them if they believe in them.


Shubham Dixit
Let me tell you something, America. You think generics are the problem? No. The problem is you’ve been brainwashed by Big Pharma’s billion-dollar ads telling you that only their logo on a pill makes it real. In India, we’ve been taking generics since the 1980s-life-saving ones, cancer drugs, HIV cocktails-and we never had this ‘psychological crisis.’ Why? Because we don’t worship brands. We care about results. A pill is a pill. If it saves your life, who cares if it’s white or has a weird logo? Your ‘nocebo effect’ is just privilege talking. We don’t have the luxury of believing in magic pills. We take what works. And guess what? We live longer than you do on less. Stop blaming your mind. Start blaming your marketing culture.
And don’t give me that ‘individualist society’ nonsense. We’re collectivist in values but individualist in action-because survival demands it. You cry about trust? We built trust by making generics affordable for millions. You? You cry about $40 vs $4. Pathetic.