When you get a vaccine, your body learns how to fight off a virus. But for a tiny number of people, something unexpected happens - their body reacts badly. Not because the vaccine doesn’t work, but because of a rare allergic response. It sounds scary, but here’s the truth: vaccine allergic reactions are extremely rare. Far rarer than being struck by lightning. And the systems in place to catch and manage them are more advanced than ever.
How Rare Are Vaccine Allergic Reactions?
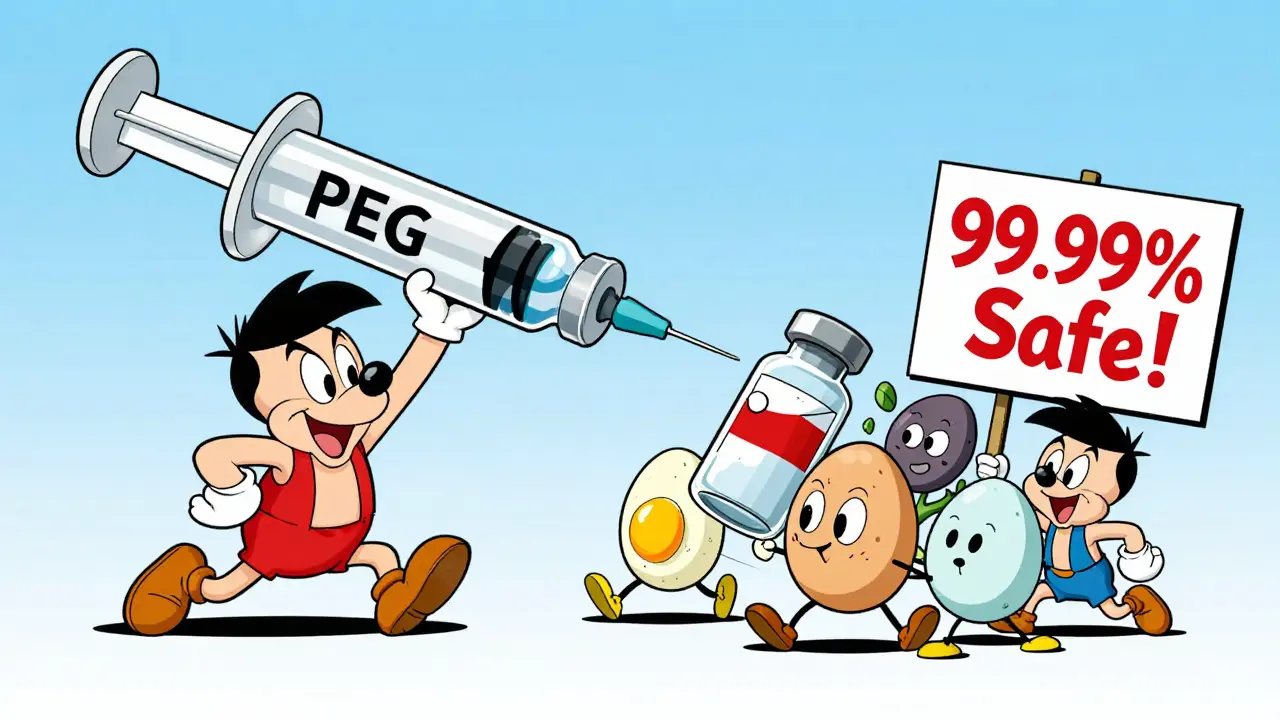
Let’s put numbers to fear. Across all vaccines given in the U.S., anaphylaxis - the most serious type of allergic reaction - happens about 1.3 times per million doses. That’s less than one in a million. For mRNA COVID-19 vaccines, the rate was slightly higher at 11.1 cases per million doses. Still, that means over 99.99% of people who get these vaccines have no allergic reaction at all.
Think about it: if 100,000 people got vaccinated, you’d expect maybe one reaction. In a city like Perth, with over two million people, that’s still just a handful of cases every year. Most reactions happen within minutes - 71% within the first 15 minutes. That’s why clinics ask you to wait 15 to 30 minutes after getting your shot. It’s not because they think you’ll react - it’s because they’re ready if you do.
What Does a Vaccine Allergic Reaction Look Like?
Not all reactions are the same. True allergic reactions are immediate and involve the immune system. The most common signs are:
- Hives or raised, itchy welts on the skin
- Swelling of the lips, tongue, or throat
- Difficulty breathing or wheezing
- Dizziness or a sudden drop in blood pressure
- Nausea or vomiting
These symptoms usually show up fast - within minutes. That’s different from common side effects like sore arms, mild fever, or fatigue. Those are normal. They don’t mean you’re allergic. They mean your immune system is doing its job.
Some people report rashes or itching hours or even days later. These aren’t true allergies. They’re often just irritation or a delayed immune response. No treatment needed. No reason to skip future vaccines.
What Causes These Reactions?
It’s not the virus or bacteria in the vaccine. Those are harmless fragments. The real culprits are usually trace ingredients:
- Polyethylene glycol (PEG): Found in mRNA vaccines like Pfizer and Moderna. It’s used to stabilize the lipid nanoparticles that carry the genetic material. A small number of people have pre-existing allergies to PEG, which is also in some laxatives and cosmetics.
- Polysorbate 80: Used in some vaccines like Johnson & Johnson’s. It’s chemically similar to PEG, so people allergic to one may react to the other.
- Egg proteins: Older vaccines (like flu shots) were made using chicken eggs. But today, even people with severe egg allergies can safely get the flu shot. Studies show over 4,300 egg-allergic individuals received flu vaccines with zero serious reactions.
- Yeast proteins: Used in some vaccines like hepatitis B and HPV. Only about 15 possible cases were ever reported in VAERS out of 180,000 allergy reports - and even those weren’t confirmed.
- Aluminum salts: These are adjuvants that help boost the immune response. They don’t cause anaphylaxis. But they can cause small, long-lasting lumps under the skin - harmless, though sometimes annoying.
Here’s the kicker: 81% of people who had allergic reactions to vaccines had a history of other allergies - asthma, food allergies, eczema, or prior anaphylaxis. That doesn’t mean vaccines are dangerous for them. It just means they’re more likely to have a reaction if they’re allergic to one of the ingredients.
How Do We Know When Something Goes Wrong?
The U.S. has a system called VAERS - the Vaccine Adverse Event Reporting System. It’s not perfect. Anyone can report anything. A headache after a shot? Reported. A fever? Reported. But here’s what makes it powerful: it catches patterns.
When the COVID-19 vaccines rolled out, VAERS picked up a spike in anaphylaxis cases. That didn’t mean the vaccines were unsafe. It meant we now had enough data to say: yes, there’s a slightly higher rate, but it’s still extremely rare. And we now know exactly what to look for - PEG allergies.
Other countries have similar systems. The European Medicines Agency’s EudraVigilance handles over 1.5 million reports a year. Australia’s TGA runs its own system. These aren’t just databases - they’re early warning networks. If a pattern emerges - say, more reactions to a new batch of a vaccine - regulators can pause use, investigate, and act.
What Happens If You Have a Reaction?
Every clinic that gives vaccines must have epinephrine on hand. That’s the only thing that stops anaphylaxis from becoming deadly. Epinephrine works fast - it tightens blood vessels, opens airways, and reverses swelling. It’s not a cure-all, but it’s the best tool we have.
After a reaction, you’re usually referred to an allergist. They’ll do tests - skin prick tests, blood tests - to see if you’re allergic to PEG, polysorbate, or another component. If you are, they’ll help you figure out which vaccines are safe. Sometimes, you can still get vaccinated using a different brand. For example, if you reacted to Pfizer’s mRNA vaccine, you might safely get Moderna’s - or even a non-mRNA option like Novavax.
And here’s the good news: even if you had a reaction to your first dose, you can often safely get a second. Studies show most people who had a mild reaction to the first shot didn’t react at all to the second - especially if they were monitored and given antihistamines beforehand.

What About Egg Allergies? Do I Still Need to Avoid Flu Shots?
No. Not anymore. This used to be a big deal. Back in the 1990s, doctors told egg-allergic people to avoid flu shots. But science changed. Research showed the tiny amount of egg protein left in modern flu vaccines doesn’t trigger reactions - even in people who’ve gone into anaphylaxis from eating egg.
Over 28 studies, involving more than 4,300 egg-allergic people, found zero serious reactions. The CDC, the American Academy of Pediatrics, and the WHO all say: no special precautions needed. No skin testing. No waiting longer. Just get the shot like anyone else.
What Should You Do Before Getting Vaccinated?
If you’ve never had a serious allergic reaction to anything - no anaphylaxis, no EpiPen use - you don’t need to do anything special. Just show up. Tell the nurse if you’ve ever had a bad reaction to a vaccine before.
If you have a history of severe allergies - especially anaphylaxis - talk to your doctor. You don’t need to avoid vaccines. But it helps to:
- Know which ingredients you’re allergic to
- Bring your EpiPen (if you have one)
- Ask if the vaccine you’re getting contains PEG or polysorbate
- Stay for the full 30-minute observation period
Don’t skip vaccines because you’re scared of a reaction. The risk of getting sick from measles, flu, or COVID-19 is thousands of times higher than the risk of an allergic reaction.
What’s Next for Vaccine Safety?
Scientists are working on better ways to predict who might react. Right now, we rely on history - if you’ve had anaphylaxis before, you’re monitored more closely. But future tools might change that.
A trial called NCT04976276 is testing skin tests for PEG and polysorbate. If it works, we could screen people before they even get the shot. Another study in Nature Immunology found a possible biomarker in mast cells - the cells that trigger allergic reactions. In five to seven years, we might have a blood test that shows if someone’s at risk.
The CDC’s 2023-2027 strategy is clear: improve detection of rare reactions. $28 million is being invested in better data tools. That means faster alerts, smarter analysis, and even better safety.
One thing won’t change: vaccines are still one of the safest medical interventions ever created. The benefits far, far outweigh the risks. And the systems watching over them? They’re working.
Can you die from a vaccine allergic reaction?
Death from a vaccine allergic reaction is extraordinarily rare. Out of more than 10 million doses studied in one major report, zero deaths occurred from allergic reactions. Epinephrine, when given quickly, is nearly always effective. Clinics are required to have it on hand, and staff are trained to use it. The risk of dying from the diseases vaccines prevent - like measles, polio, or COVID-19 - is vastly higher.
If I had a reaction to one vaccine, does that mean I can’t get others?
Not necessarily. Reactions are usually tied to specific ingredients, not vaccines as a whole. For example, if you reacted to an mRNA vaccine because of PEG, you might still safely receive a non-mRNA vaccine like Novavax. Or if you reacted to the flu shot because of a preservative, you could try a different brand. An allergist can help you figure out what’s safe.
Are children at higher risk for vaccine allergies?
No. Most reactions occur in adults, especially women over 40. Among children and teens, the rate is about 0.22 per 100,000 doses - even lower than in adults. Kids with egg allergies can safely get the MMR vaccine. There’s no evidence that childhood vaccines are more likely to cause allergic reactions than adult ones.
Why do so many people think vaccines cause allergies?
It’s mostly because rare events get attention. If 10 million people get vaccinated and one has a reaction, that one case makes headlines. Meanwhile, the 9.9 million who had no reaction don’t make news. Social media amplifies fear. But data shows the risk is minimal. Vaccine hesitancy due to allergy fears accounts for only about 12% of cases - and most of those fears are based on outdated info.
Should I avoid vaccines if I have a history of anaphylaxis?
No. Anaphylaxis to other things - like peanuts, bee stings, or penicillin - doesn’t mean you can’t get vaccines. Unless you know you’re allergic to a specific vaccine ingredient (like PEG), you should still get vaccinated. Talk to your doctor or allergist first. They can help you choose the safest option and manage the process.


Agnes Miller
Just got my booster yesterday and was nervous as hell, but the nurse walked me through everything. Said they keep epinephrine right by the chair and watch you like a hawk for 30 mins. Honestly? Felt safer than going to the ER. The stats they gave me? Mind-blowing. 1 in a million? I’d take those odds over getting the flu any day.