Drug Rash Severity Checker
This tool helps you understand if your rash might be serious. It is not a medical diagnosis. Always consult your doctor or go to ER for serious symptoms.
When you start a new medication, you expect it to help - not make your skin angry. But if you’ve ever noticed red bumps, itching, or patches of flaky skin after taking a pill, you’re not alone. Around 2-5% of all drug reactions involve the skin, and for many, it’s the first sign something’s off. These aren’t just annoyances. Some rashes are harmless and fade on their own. Others? They can be life-threatening. Knowing the difference could save your life.
What Does a Drug Rash Look Like?
Not all skin reactions are the same. The most common type is a morbilliform rash - think measles-like spots that spread symmetrically across your chest, back, or arms. It usually shows up 4 to 14 days after starting a new drug, though it can appear sooner if you’ve taken it before. It’s often itchy, sometimes accompanied by a low fever. The good news? About 90% of these cases clear up within one to two weeks after stopping the medication. Then there’s urticaria, or hives. These are raised, red, swollen welts that come and go, sometimes within hours. They’re often tied to allergic reactions and usually fade within 24 to 48 hours after you stop the drug. But if hives are paired with swelling of the lips, tongue, or throat - or trouble breathing - that’s an emergency. Call for help immediately. Another type is nummular dermatitis. It looks like coin-shaped, dry, scaly patches on the arms, legs, or torso. It’s often mistaken for eczema, but if it appeared right after starting a new medication, it’s likely drug-induced. These patches clear faster than regular eczema - usually within 4 to 8 weeks - once the drug is stopped.The Dangerous Ones You Can’t Ignore
Most drug rashes are mild. But a small fraction - less than 2% - are severe and can be deadly. These include:- Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN): These start like a flu, then blistering spreads across the skin and mucous membranes (mouth, eyes, genitals). SJS has a 5-15% death rate. TEN, the more severe form, kills 25-35% of those affected. If you notice skin peeling off in large sheets or painful sores in your mouth, get to an ER now.
- DRESS syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms): This one sneaks up. It can take 2 to 6 weeks after starting a drug to show up. Symptoms include fever, swollen lymph nodes, liver inflammation, and a widespread rash. Blood tests will show high eosinophils. Common culprits? Carbamazepine, phenytoin, lamotrigine, allopurinol, and sulfonamides. Treatment often needs weeks of steroids and hospital care.
- Acute Generalized Exanthematous Pustulosis (AGEP): This looks like small, pus-filled bumps covering large areas of skin. It’s rare but often linked to antibiotics like minocycline or antifungals. Usually resolves within days of stopping the drug.
These severe reactions - SJS, TEN, DRESS, and AGEP - account for 90% of all drug rash deaths. That’s why early recognition matters more than you think.
Which Medications Cause the Most Reactions?
Some drugs are notorious for skin reactions. Based on data from US Pharmacist and the Mayo Clinic:- Penicillins - cause about 10% of all drug rashes. Penicillin allergies are the most common drug allergy, but here’s the twist: 15% of people who think they’re allergic to penicillin aren’t. Skin testing now identifies true allergies with 95% accuracy.
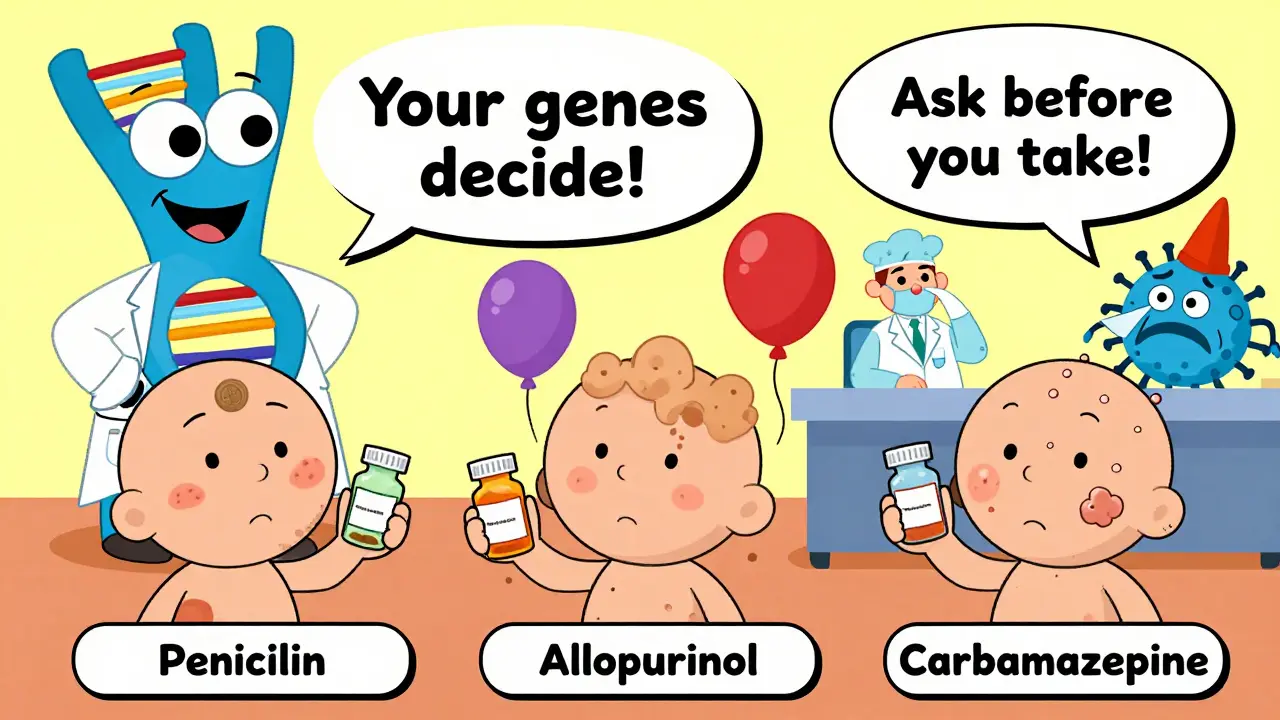
- Anticonvulsants - carbamazepine, phenytoin, lamotrigine. These are the top triggers for DRESS and SJS. In Southeast Asia, people with the HLA-B*1502 gene are 1,000 times more likely to get SJS from carbamazepine. Testing for this gene is routine in some countries before prescribing.
- Allopurinol - used for gout. In Han Chinese populations, those with the HLA-B*5801 gene have a 580-fold higher risk of severe reactions. Again, genetic screening is available.
- NSAIDs - like ibuprofen and naproxen. These often cause non-allergic reactions - not immune-related, but still irritating. About 25% of non-allergic drug rashes come from these.
- Antibiotics - especially sulfonamides (Bactrim) and minocycline. If you have a viral infection like mono or HIV and take an antibiotic, your risk of a severe rash jumps 5 to 10 times.
Why Some People React - And Others Don’t
It’s not random. Your genes play a huge role. If you’re from Southeast Asia, your risk of SJS from carbamazepine is higher. If you’re Han Chinese, allopurinol could be dangerous. These aren’t guesses - they’re genetic facts backed by research. Also, your immune system might already be primed. Ever taken a drug years ago and had no reaction? You could’ve been sensitized then. Tiny amounts in food, or even past exposures, can train your body to react later. That’s why some people develop allergies after years of safe use. And if you’re older? Taking five or more medications? Your lifetime risk of a drug rash jumps to 35%. For someone on one or two drugs? It’s only 5%. Polypharmacy isn’t just about drug interactions - it’s about skin reactions too.What to Do If You Get a Rash
Don’t panic. But don’t ignore it either.- Don’t stop your medication on your own. Especially if it’s for seizures, high blood pressure, or heart disease. Stopping suddenly could be worse than the rash. Call your doctor.
- Take a photo. Skin rashes change fast. A photo helps your doctor track it.
- Write down everything. What drug did you start? When? What else are you taking? Did you have a viral infection recently? Even a cold can raise your risk.
- Watch for red flags. If you have fever, blistering, peeling skin, mouth sores, swelling, or trouble breathing - go to the ER. Don’t wait.
For mild rashes, your doctor might suggest:
- Lukewarm baths with fragrance-free cleansers
- Applying emollients (like CeraVe or Eucerin) within 3 minutes of bathing
- Over-the-counter hydrocortisone 1% cream twice daily
For more serious cases, you might need prescription creams like clobetasol 0.05% or oral steroids like prednisone. DRESS syndrome often requires weeks of treatment. SJS/TEN? That’s ICU-level care.
How to Prevent Future Reactions
- Know your triggers. If you’ve had a reaction to a drug, write it down. Include the name, date, and symptoms. Share this with every doctor you see.
- Ask about alternatives. If you’re prescribed penicillin and you think you’re allergic, ask if you can be tested. Many people aren’t truly allergic.
- Be cautious with new drugs. If you’re starting a new medication, watch your skin closely for the first two weeks.
- Check for photosensitivity. Some drugs - like doxycycline, ciprofloxacin, or hydrochlorothiazide - make your skin burn easily in the sun. Wear sunscreen and cover up.
There’s no way to guarantee you’ll never get a drug rash. But you can reduce your risk. Keep a list of all your medications. Talk to your pharmacist. And if something feels off - trust your skin. It’s telling you something.
What’s Changing in Diagnosis and Treatment
Doctors are getting better at spotting these reactions. Skin testing for penicillin allergies is now accurate enough to rule out false positives. Genetic testing for HLA-B*1502 and HLA-B*5801 is being used before prescribing certain drugs in high-risk populations. And hospitals are using multidisciplinary teams - dermatologists, pharmacists, intensivists - to manage severe cases. But the biggest shift? Recognizing that not all rashes are allergic. Many are just toxic reactions. That changes how you treat them. Steroids might help one type, but not another. Misdiagnosing nummular dermatitis as eczema can delay recovery by months.Final Takeaway
Skin rashes from medications are common - but not always harmless. Most are mild and go away. But a few can be deadly. If you notice new redness, bumps, or peeling after starting a drug, pay attention. Don’t assume it’s just a bug or dry skin. Talk to your doctor. Keep track. And never ignore symptoms that worsen or spread.Your skin is a mirror. When it reacts, it’s not just a side effect - it’s a signal. Learn to read it.
Can a drug rash appear weeks after starting a medication?
Yes. While many rashes appear within days, some take weeks. DRESS syndrome, for example, usually shows up 2 to 6 weeks after starting the drug. Even if you’ve been taking a medication for a month, a new rash could still be drug-related. Don’t assume it’s something else just because you’ve been on it a while.
If I had a rash from one antibiotic, will I react to all of them?
Not necessarily. Reactions are usually specific to one drug or a closely related group. For example, if you reacted to amoxicillin, you might still tolerate cephalexin - but you shouldn’t assume that. Always check with your doctor before trying another antibiotic. Cross-reactivity is possible but not guaranteed.
Can I be tested for drug allergies like I can for food allergies?
Only for a few drugs. Penicillin is the most common one with reliable skin testing - it’s over 95% accurate. For others, like sulfa drugs or NSAIDs, testing isn’t standardized. Diagnosis usually relies on your history, timing of the reaction, and ruling out other causes. Genetic testing is available for specific drugs like carbamazepine and allopurinol if you’re in a high-risk group.
Is it safe to take a drug again if I had a mild rash before?
Generally, no. Even if your rash was mild, re-exposure can lead to a much worse reaction. The immune system remembers. If you had a morbilliform rash, your doctor might consider a graded challenge under supervision - but only if the drug is essential and no alternatives exist. Never try it on your own.
Do over-the-counter creams help with drug rashes?
For mild, non-blistering rashes, yes - hydrocortisone 1% cream and moisturizers can help reduce itching and inflammation. But if the rash is spreading, blistering, or painful, OTC creams won’t help. That’s a sign you need medical evaluation. Don’t delay treatment for serious reactions hoping a cream will fix it.
Can a drug rash be mistaken for an infection?
Yes, often. Viral infections like Epstein-Barr (mono) or HIV can cause rashes that look exactly like drug reactions - especially when antibiotics are taken at the same time. Doctors look for clues: Did the rash appear after the drug? Are there other symptoms like fever or swollen glands? Blood tests and timing help tell the difference.
If you’ve had a drug rash before, keep a written record. Include the drug name, date, symptoms, and what happened after. Share this with every healthcare provider you see. Your skin remembers - and so should you.

