Every year, millions of people in the U.S. pay hundreds of dollars for prescriptions they could get for under $10. The difference? Generic medications. If you’ve ever looked at your pharmacy receipt and wondered why your blood pressure pill costs $4 instead of $130, you’re not alone. Most people assume the cheaper version must be weaker, less safe, or somehow inferior. But that’s not true. Generic drugs are not a compromise-they’re the same medicine, approved by the same agency, and backed by decades of real-world evidence.
They’re the exact same drug, legally required to be
The U.S. Food and Drug Administration (FDA) doesn’t approve generics lightly. To be sold, a generic drug must contain the same active ingredient, in the same strength, and delivered the same way (pill, injection, inhaler, etc.) as the brand-name version. It must also work the same way in your body. That’s not marketing speak-it’s a legal requirement. The FDA demands proof through bioequivalence studies, which show the generic delivers the same amount of medicine into your bloodstream at the same rate as the brand. The acceptable range? Between 80% and 125% of the brand’s performance. That’s tight enough to ensure no meaningful difference in how the drug works.Cost savings aren’t just nice-they’re life-changing
The biggest reason to switch? Money. Plain and simple. Generic drugs cost, on average, 80-85% less than their brand-name equivalents. For example, the cholesterol-lowering drug Lipitor (atorvastatin) used to cost over $130 a month. Today, the generic version? As low as $4 at major pharmacies. Warfarin, a blood thinner, used to be sold as Coumadin for over $300 a month. The generic? Around $4. Same pill. Same effect. Same safety record. These aren’t outliers. A 2023 FDA report showed that when five or more companies make the same generic drug, prices drop by nearly 85%. That’s competition at work. And it’s not just individuals saving money-it’s the whole system. From 2012 to 2022, generic drugs saved the U.S. healthcare system over $1.67 trillion. That’s enough to cover the annual healthcare costs for nearly 50 million people.Insurance plans push generics for a reason
If you’re on insurance, you’ve probably noticed your copay is $1-$10 for generics but $25-$75 for brand-name drugs. That’s not an accident. Insurance companies use tiered formularies to steer patients toward generics because they know the clinical outcomes are identical. For Medicare Part D beneficiaries in 2023, the average copay for a generic was $1.85. For a brand-name drug? $33.67. That’s nearly 18 times more. Many plans require you to try the generic first before approving the brand. This isn’t about saving the insurer money-it’s about saving you money. And if the generic doesn’t work for you? You can appeal. But in most cases, it does.They’re just as safe-maybe even safer
Some people worry that because generics are cheaper, they’re made in lower-quality facilities. That’s a myth. The FDA inspects all manufacturing plants-brand and generic alike-with the same standards. In fact, many brand-name companies make their own generics after the patent expires. The FDA conducted over 1,200 inspections of generic drug facilities in 2023 alone. And here’s the kicker: adverse event reports for generics are proportional to their usage. Since generics make up 90% of all prescriptions, they naturally show up more in safety reports. But the rate of problems? No different from brand-name drugs. A 2022 study in the Journal of Managed Care & Specialty Pharmacy looked at over 186,000 patients on heart medications. The results? No difference in effectiveness or safety between generic and brand-name versions. Same for diabetes, high blood pressure, depression, and thyroid meds. The American Medical Association recommends prescribing generics whenever possible-not because they’re cheaper, but because they’re just as effective.
What about those weird-looking pills?
You might notice your pill changed color, shape, or size. That’s because generic manufacturers use different inactive ingredients-fillers, dyes, coatings-that don’t affect how the drug works. The FDA allows these differences because they don’t impact safety or effectiveness. But they can cause anxiety. One patient on Reddit said, “My pharmacy switched generic brands and the pill turned from blue to white. I thought I was getting the wrong medicine.” That’s a psychological issue, not a medical one. Pharmacists are trained to explain this. Ask them. Read the label. Check the active ingredient. If it matches what your doctor prescribed, you’re fine. If you’re still uneasy, ask for the same manufacturer. Many pharmacies let you request a specific generic brand.What about special cases? Epilepsy, thyroid, blood thinners?
Some doctors are cautious with drugs that have a narrow therapeutic index-medications where even a small change in blood level can cause problems. Think warfarin, levothyroxine, or certain seizure drugs. For these, the FDA still requires the same bioequivalence standards. But some clinicians prefer to stick with one manufacturer if a patient is stable. That doesn’t mean generics are unsafe. It means consistency matters. If you’re doing well on a specific generic, don’t switch unless you have to. But if you’re starting a new medication, the generic is still the right first choice. The FDA has approved hundreds of generics for these drugs, and studies show no increase in hospitalizations or side effects.Real people, real savings
A diabetes patient on PatientsLikeMe wrote: “Metformin generics cost me $4 a month. Glucophage was $300. This keeps me on my meds.” A man on Reddit shared: “Switching my blood pressure meds to generic saved me $280 a month. No side effects. Just lower bills.” Kaiser Permanente’s 2023 survey found 87% of patients were satisfied with generics. The top reason? Affordability. And here’s the most powerful stat: patients using generics are 68% less likely to skip doses because of cost. That’s not just savings-it’s better health outcomes.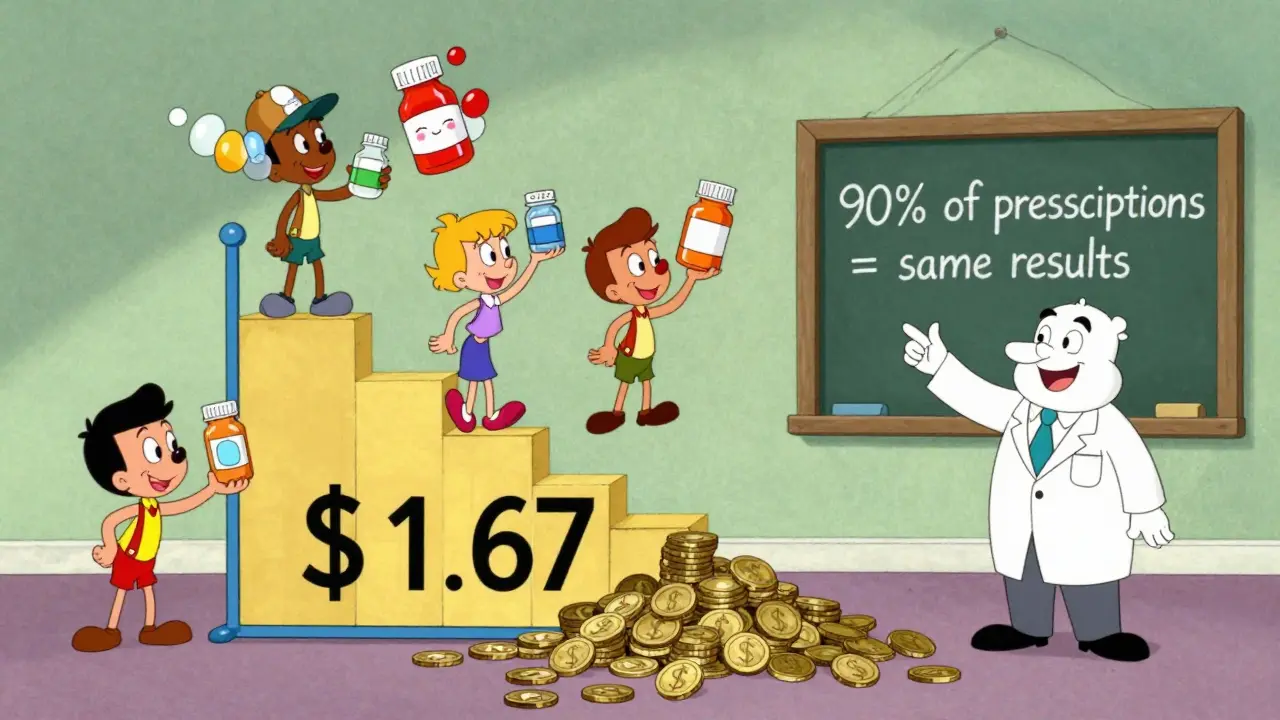
How to switch
Switching is simple:- Ask your doctor: “Is there a generic for this?”
- If yes, ask your pharmacist: “Can you fill this with the generic?”
- Check your insurance formulary-generics are almost always tier 1.
- Don’t panic if the pill looks different. Check the label for the active ingredient.
- If you feel something’s off, call your doctor. But don’t assume it’s the generic’s fault.
What’s next? Biosimilars and more savings
The next wave is biosimilars-generic versions of complex biologic drugs like Humira or Enbrel. These used to cost $20,000 a year. Now, biosimilars are hitting the market at 15-35% less. The Congressional Budget Office estimates they’ll save Medicare $50 billion annually by 2030. This isn’t the future-it’s happening now.Bottom line: Don’t pay more for the same thing
There’s no medical reason to pay 8-10 times more for a brand-name drug when the generic does the exact same job. The FDA, the AMA, insurers, hospitals, and millions of patients agree: generics are safe, effective, and essential. If your doctor hasn’t mentioned generics, ask. If your pharmacist switches you without telling you, ask why. But don’t let fear or habit cost you hundreds-or thousands-every year.You’re not getting a cheaper version. You’re getting the same medicine, at a fraction of the price. And that’s not just smart. It’s responsible.


Siobhan Goggin
Switched my statin to generic last year and haven’t looked back. Same pill, same results, $120 less per month. Simple math.