When a patient walks into your office with a prescription for a brand-name drug, and you know there’s a cheaper generic version available, what do you do? For many providers, it’s not just about cost-it’s about trust, consistency, and clinical outcomes. Over the last two decades, generic medications have gone from being seen as a budget alternative to becoming the backbone of affordable care. But behind the statistics-90% of prescriptions filled, only 23% of spending-are real stories from doctors, pharmacists, and clinics navigating the messy reality of switching patients from brand to generic.
It’s Not Just About Price
Most providers agree: generics save money. A statin like atorvastatin costs $4 a month as a generic versus $150 for Lipitor. That’s not a small difference. For a patient on fixed income, that gap means they either take the medicine or skip it. Studies show patients who start on generics are 13% more likely to stick with their treatment long-term. But cost isn’t the whole story. One GP in Ohio told me about a 68-year-old woman with high blood pressure who kept showing up with uncontrolled readings. Turns out, she was switching between three different generic brands every month because her pharmacy changed suppliers. She didn’t know they were supposed to be the same. She thought each one was a different drug. That confusion? It’s more common than you think.When Generics Work-And When They Don’t
For most medications, the switch is seamless. Antibiotics, blood pressure pills, antidepressants like sertraline, and even diabetes meds like metformin have been used in generics for years with no measurable drop in effectiveness. A 2019 JAMA study tracked over 10 drugs-some with authorized generics (made by the original brand) and others by third-party manufacturers. No difference in hospitalizations. No difference in whether patients stopped taking them. The FDA’s bioequivalence standards are strict: generics must deliver the same amount of active ingredient into the bloodstream within the same time window as the brand. That’s not a guess. It’s lab-tested, peer-reviewed science. But then there are the exceptions. Antiepileptic drugs like lamotrigine. Immunosuppressants like tacrolimus after a kidney transplant. Warfarin for blood thinning. These are narrow therapeutic index drugs. That means the difference between a dose that works and one that causes harm is tiny. Providers in transplant centers and neurology clinics report cases where patients had breakthrough seizures or rejected a transplanted organ after switching to a generic. In one documented case, a patient on brand-name lamotrigine for 12 years had a seizure two weeks after switching to a generic. Switching back to the brand? Seizures stopped. That’s not rare. It’s enough that the American College of Neurology says: don’t automatically substitute AEDs without patient and provider consent.The Concerta Case That Changed Everything
In 2016, the FDA did something unusual. They changed the therapeutic equivalence rating for two generic versions of Concerta, a popular ADHD medication, from AB (therapeutically equivalent) to BX (not equivalent). Why? Because patients and providers were reporting that the generics weren’t working. Not just complaints-real data. The FDA reviewed adverse event reports, tested the pills in labs, and analyzed how the drug released in the body. Turns out, the generic versions released the active ingredient too quickly. For a drug designed to work over 12 hours, that’s a big deal. Kids were losing focus by lunchtime. Parents were calling schools. Teachers noticed changes. The FDA didn’t just rely on bioequivalence studies-they looked at what was happening in real life. That case became a turning point. Providers now know: not all generics are created equal, even if they’re labeled the same.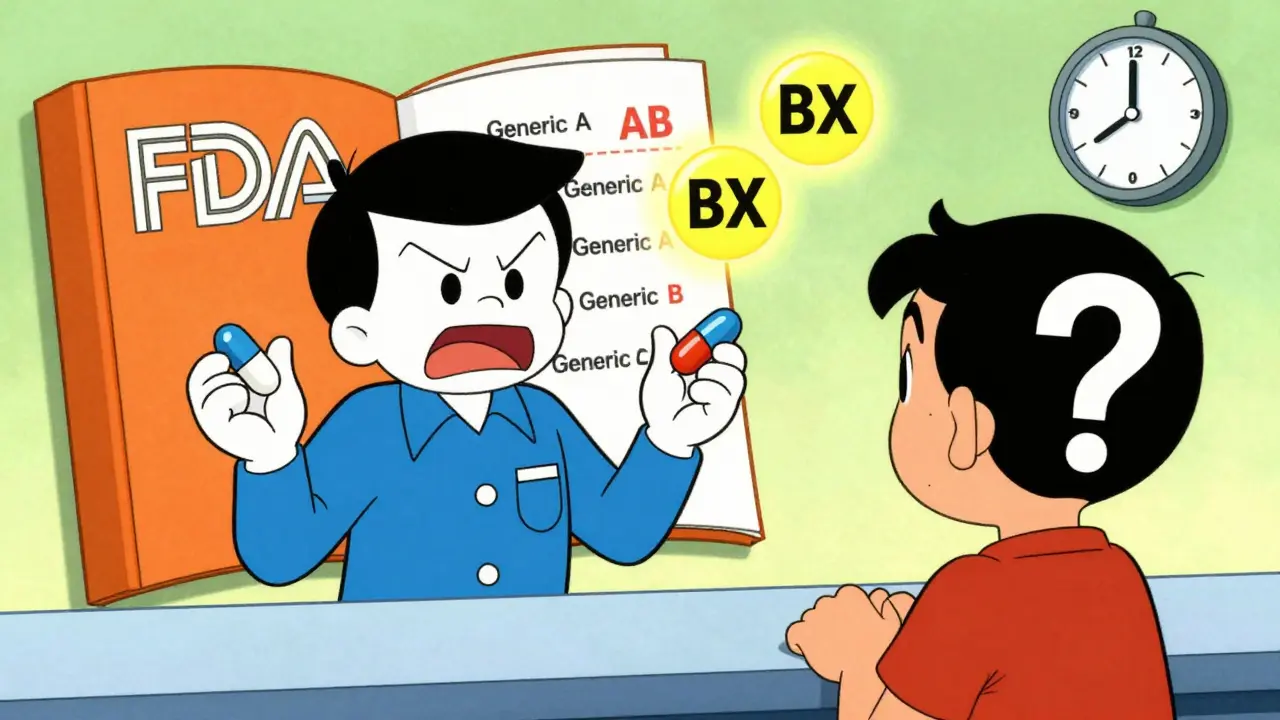
State Rules Are a Patchwork
You’d think the rules for switching to generics would be the same everywhere. They’re not. In 19 states, pharmacists can automatically substitute a generic unless the doctor writes “dispense as written.” In seven states and Washington, D.C., the pharmacist must get the patient’s permission first. And 24 states don’t protect pharmacists from liability if something goes wrong after a switch. That means some pharmacists are scared to substitute, even when it’s safe. One pharmacist in Florida told me she avoids substituting for any drug with a narrow therapeutic index unless the doctor specifically says it’s okay. She doesn’t want to be the one blamed if a patient has a bad reaction. Electronic health records help. Many now flag whether a drug is AB-rated or BX-rated in the FDA’s Orange Book. But not all systems are updated. Some still show “generic” without the rating. That’s dangerous. Providers need to know the difference. If a patient is on warfarin and gets switched to a BX-rated generic, that’s a red flag. That’s not just a cost-saving move-it’s a clinical risk.Patients Believe What They’re Told
A 2024 survey in Greece found that 68% of women followed their doctor’s advice to switch to generics. Only 64% of men did. Why? Because women were more likely to have had a conversation about it. The key isn’t the drug. It’s the conversation. When providers take two minutes to explain that generics have the same active ingredient, same FDA approval, and same safety profile-adherence goes up. Patients stop worrying about “cheap” or “inferior.” They start trusting the system. One endocrinologist in Minnesota started including a printed one-pager in every prescription for levothyroxine. It explained bioequivalence, why generics are safe, and what to do if symptoms changed. Within six months, patient questions about the switch dropped by 70%. But misinformation still spreads. Some patients believe generics are made in “lesser” factories. The truth? Many brand-name drugs and generics come from the same plants. The FDA inspects them all. The difference is in the name on the box, not the pill inside.Authorized Generics: The Hidden Middle Ground
There’s another option many don’t know about: authorized generics. These are the exact same pills as the brand-name drug, just sold without the brand name. Made by the original company. Same factory. Same packaging, just a different label. They’re often priced between the brand and the regular generic. For providers who want to reduce cost but are nervous about switching, authorized generics are a smart middle ground. They’re especially useful for patients on complex drugs like inhalers or long-acting injectables, where formulation differences matter more.
What Providers Are Doing Differently Now
The most experienced providers have learned to treat generics like any other clinical decision. They don’t assume. They assess.- For chronic, stable conditions like hypertension or high cholesterol? Switch freely. The data supports it.
- For epilepsy, transplant meds, or anticoagulants? Always check the Orange Book rating. Use AB-rated only. Consider authorized generics if available.
- For patients with a history of switching and relapse? Write “dispense as written.” Don’t wait for a crisis.
- For patients who are confused or anxious? Explain it. A two-minute conversation beats a hundred pages of pamphlets.
The Bigger Picture
Generics aren’t perfect. But they’re the best tool we have to make medicine affordable without sacrificing safety. The FDA approved 745 generic drugs in 2022. That’s more than ever. The Inflation Reduction Act is pushing Medicare to favor generics even more. By 2025, we could see a 5-7% jump in generic use. That’s billions saved. But savings mean nothing if patients stop taking their meds because they’re confused, scared, or got the wrong version. The real win isn’t in the price tag. It’s in the conversation. It’s in knowing when to switch-and when to hold back. It’s in listening to patients who say, “This one doesn’t feel right.” And then having the data, the tools, and the courage to act on it.What Comes Next
Machine learning is starting to help. A 2024 study in Greece used AI to predict which patients were most likely to have trouble switching to generics. Factors? Age, education, previous adverse reactions, and how many times they’d switched before. The model was 82% accurate. Imagine a system that flags high-risk patients before the pharmacist even fills the script. That’s not science fiction. It’s coming. The supply chain is still fragile. Eighty percent of active ingredients come from outside the U.S. That’s a risk. But the FDA is pushing for more domestic manufacturing. And with new guidance on complex generics-like inhalers and topical creams-the approval process is getting smarter. The message is clear: generics work for most people, most of the time. But they’re not one-size-fits-all. The provider’s job isn’t just to prescribe. It’s to guide.Are generic medications as effective as brand-name drugs?
For the vast majority of medications, yes. The FDA requires generics to prove they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand. Studies show no difference in outcomes for drugs like statins, blood pressure meds, and antidepressants. But for narrow therapeutic index drugs-like warfarin, thyroid meds, or antiepileptics-substitution can sometimes cause issues. Always check the FDA’s Orange Book for the therapeutic equivalence rating (AB = safe to substitute, BX = not recommended).
Why do some patients have problems after switching to generics?
It’s usually not the active ingredient-it’s the formulation. Generics can have different fillers, coatings, or release mechanisms. For most drugs, this doesn’t matter. But for drugs where timing is critical-like extended-release ADHD meds or seizure drugs-even small changes can affect how the body absorbs the medicine. In rare cases, patients report feeling different after a switch. That’s why providers now check for FDA’s BX ratings and ask patients if they’ve had issues before.
Can pharmacists switch my prescription without telling me?
It depends on your state. In 19 states, pharmacists can substitute generics automatically unless the doctor says “dispense as written.” In seven states and D.C., they must get your permission first. Some states don’t protect pharmacists from liability, so they may avoid substitution altogether. Always ask if a generic was substituted-and if you’re on a sensitive medication like warfarin or lamotrigine, insist on knowing the brand or generic version you’re getting.
What’s the difference between a generic and an authorized generic?
An authorized generic is made by the same company that makes the brand-name drug, just sold without the brand name. It’s identical in every way-same factory, same ingredients, same packaging except for the label. A regular generic is made by a different company, even if it meets FDA standards. Authorized generics are often a safer choice for patients on complex or narrow therapeutic index drugs because there’s zero change in formulation.
How can I tell if a generic is safe to use?
Check the FDA’s Orange Book online or ask your pharmacist. Look for an “AB” rating-that means it’s approved as therapeutically equivalent. Avoid drugs with a “BX” rating unless your provider specifically approves it. Also, pay attention to changes in pill appearance or side effects after a switch. If something feels off, tell your provider. Don’t assume it’s “all in your head.”
Do generics cause more side effects than brand-name drugs?
No, not overall. Large studies show no increase in side effects from generics. But some patients report feeling different after switching, especially if they’ve been on the same brand for years. This is often due to changes in inactive ingredients (like fillers or dyes) or how the drug is released. For most people, this is harmless. For a small group on critical medications, it can be significant. That’s why provider-patient communication matters more than the pill itself.

Jocelyn Lachapelle
Generics saved my dad's life. He was on Lipitor for years, then switched to atorvastatin and never looked back. His blood pressure stabilized, and he finally started taking it daily. No more skipped doses. Just simple, affordable care. 💙