Every year, Americans spend over $700 billion on prescription drugs. But here’s the twist: 90% of the pills and injections people take aren’t the expensive brand-name versions. They’re generics. And that’s where the real savings happen.
Generic drugs aren’t cheap-they’re a lifeline
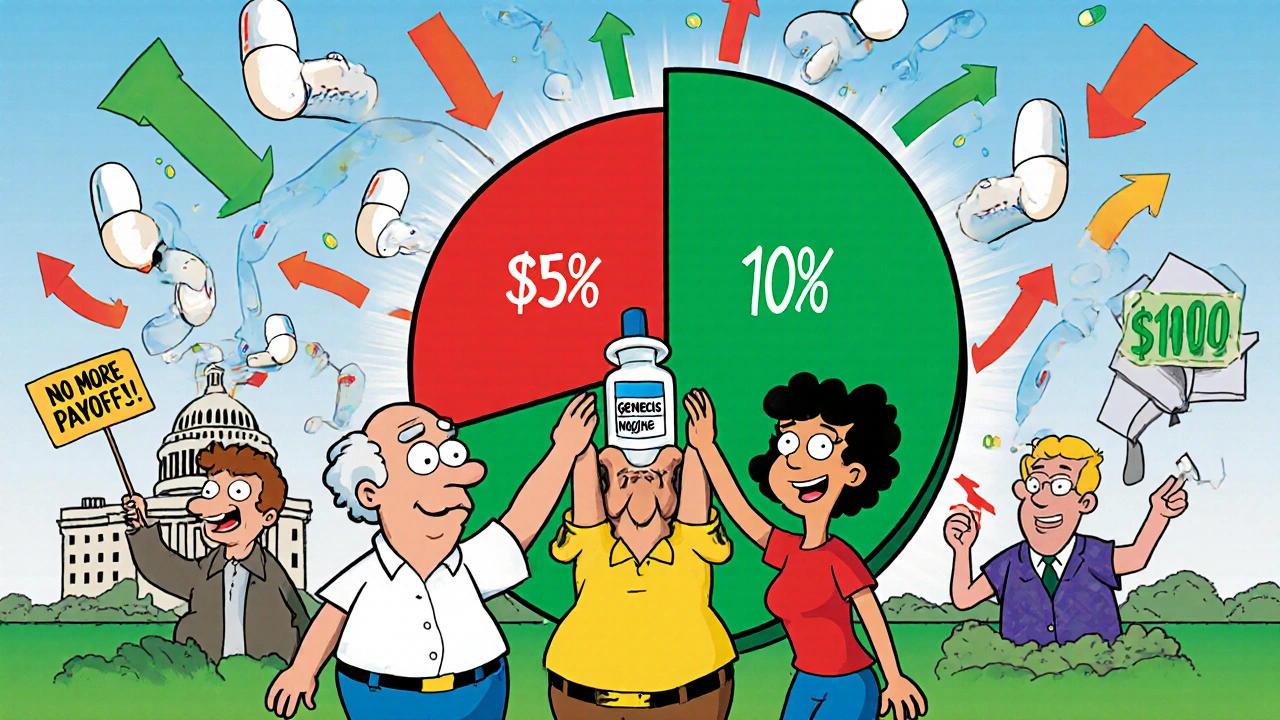
In 2024, generic medications made up 90% of all prescriptions filled in the U.S.-that’s 3.9 billion prescriptions. Yet they only cost $98 billion. Meanwhile, brand-name drugs, which made up just 10% of prescriptions, cost $700 billion. That’s not a typo. For every dollar spent on prescriptions, 88 cents went to brand-name drugs. The rest? Generics.
This isn’t magic. It’s math. Generics are chemically identical to their brand-name counterparts. They work the same way. They’re held to the same FDA standards. But because they don’t carry the cost of marketing, clinical trials, or patent protection, they cost 80-90% less. In 2024 alone, generics saved the U.S. healthcare system $482 billion. That’s more than the entire GDP of Norway.
Think about what that means for real people. A patient on a $300-a-month brand-name asthma inhaler switches to the generic version-now it’s $40. That’s $3,120 a year saved. For someone on a fixed income, that’s groceries, rent, or heating. According to GoodRx, nearly 1 in 12 Americans has medical debt because they couldn’t afford their meds. Generics are often the difference between taking your medicine and skipping it.
The biosimilar revolution-what you’re not hearing
Generics aren’t the only game in town anymore. Biosimilars are the next wave. These aren’t just copies-they’re highly similar versions of complex biologic drugs made from living cells. Think Humira, Enbrel, or Stelara. These drugs cost $70,000 a year per patient. And until recently, there was no competition.
Now, biosimilars are changing that. In 2024, Humira biosimilars went from being used in just 3% of cases to 28%. Why? Because health plans and pharmacies started pushing them. They reimbursed pharmacists fairly. They cut red tape on prior authorizations. The result? Billions saved. One major health plan saved $1.2 billion in a single year just by switching patients to Humira biosimilars.
And it’s accelerating. Stelara, a $6 billion-a-year drug, now has seven biosimilars approved. They’re priced at more than 80% less than the original. Once fully adopted, they could save $4.8 billion per year. That’s enough to cover free insulin for every Medicare beneficiary for two years.
But here’s the problem: 90% of the biologic drugs set to lose patent protection in the next 10 years have no biosimilar in development. That’s a $234 billion missed opportunity. Why? Because big pharma still holds the patents, controls distribution, and pays off competitors to delay entry. More on that later.
Why brand-name drugs cost so much
Brand-name drugs don’t cost more because they’re better. They cost more because they can. The U.S. pays more than three times what other OECD countries pay for the exact same drugs. Why? Because we don’t negotiate prices. Other countries set limits. We don’t.
Take insulin. In 2020, a vial cost $275. In 2024, after public pressure and Medicare intervention, Eli Lilly slashed the price to $25 for their non-branded version. That’s not because the cost of production dropped. It’s because the market was forced to change.
Another tactic: pay-for-delay. Big pharma pays generic manufacturers to stay off the market. In 2024, these deals cost the system an estimated $1.2 billion per year. One example? A brand-name drug manufacturer paid a generic company $100 million to delay launching a cheaper version for 18 months. During that time, patients paid $1,500 a month. After the delay ended, the generic hit the market at $40. That’s $1,460 per patient, per month, wasted-just because a deal was made behind closed doors.

How Medicare and policy are changing the game
The Inflation Reduction Act gave Medicare the power to negotiate prices for 10 drugs in 2026, ramping up to 30 per year. The Congressional Budget Office estimates this will save $500-550 billion over a decade. But that’s just the start. If those negotiated prices were extended to Medicaid and private insurers, total savings could hit $1 trillion.
And it’s working already. Medicare’s new insulin cap-$35 per month-has already cut out-of-pocket costs for seniors. By 2027, similar caps will apply to commercial insurance. That’s not just policy. That’s relief.
Even the White House is stepping in. In November 2025, Eli Lilly and Novo Nordisk agreed to cut the price of Ozempic and Wegovy from over $1,000 to $350 per month under a new Most-Favored-Nation pricing model. That’s still expensive, but it’s a sign that pressure is working.
Who benefits-and who gets left behind
Patients win. Health plans win. Employers win. Taxpayers win. But not everyone does.
Big pharma’s profits are shrinking in some areas. That’s why they’re pouring money into lobbying. In 2024, pharmaceutical companies spent over $300 million on federal lobbying. That’s more than any other industry.
And there’s still a gap. Many patients don’t know their prescription has a generic. Pharmacists can switch them automatically in some states, but not all. Some patients get switched to a different generic version that doesn’t work as well for them-especially with complex meds like seizure or psychiatric drugs. That’s not the fault of generics. It’s a failure of communication and oversight.
CMS data shows that less than 1% of Medicare beneficiaries who hit the catastrophic coverage phase use only generics. That means most are still paying for expensive brand-name drugs-even when cheaper, equally effective options exist.
What’s next? The road to trillion in savings
By 2030, if we keep expanding generic and biosimilar use, U.S. drug spending could drop by 15-18%. That’s $100-120 billion in annual savings. Add in full Medicare price negotiation, and we’re looking at over $1 trillion saved over the next decade.
But it won’t happen on its own. We need:
- Transparency: Require drug companies to disclose how they set prices.
- Enforcement: Crack down on pay-for-delay deals with real penalties.
- Access: Make sure pharmacists can substitute generics without extra paperwork.
- Investment: Fund biosimilar development for the 90% of biologics with no competition coming.
Generics aren’t a band-aid. They’re the foundation of affordable care. They’ve saved $482 billion in one year. That’s more than the entire annual budget of the Department of Education. And we’re just getting started.
Why this matters for everyone
Healthcare costs aren’t just a government problem. They’re your problem. Your premiums. Your deductible. Your co-pay. Your choice between medicine and rent.
When you ask for a generic, you’re not just saving money. You’re pushing back against a system that profits from confusion. You’re helping your neighbor afford their insulin. You’re making the system work for people, not just corporations.
There’s no magic bullet. But generics? They’re the closest thing we have.
Are generic drugs as safe and effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also meet the same strict standards for purity, stability, and performance. Bioequivalence studies prove they work the same way in the body. Millions of patients use generics every day with no difference in outcomes.
Why are biosimilars cheaper than brand-name biologics?
Biosimilars don’t need to repeat the full clinical trials that the original biologic went through. Instead, they prove they’re highly similar in structure, function, and clinical effect. This reduces development costs by 70-80%. Since multiple companies can make biosimilars for the same drug, competition drives prices down-often to 20-30% of the brand-name price.
Can I ask my doctor or pharmacist for a generic version?
Absolutely. In most cases, your doctor can prescribe a generic, and your pharmacist can substitute one unless the prescription says "dispense as written" or "no substitution." Always ask if a generic is available-it could save you hundreds or even thousands a year. If your pharmacy refuses, ask why. Sometimes it’s just a PBM policy, not a medical reason.
Do generics cause more side effects than brand-name drugs?
No. The FDA monitors adverse events for both brand-name and generic drugs equally. Studies show no difference in side effect rates. Sometimes, patients report differences-but that’s often due to inactive ingredients (like fillers or dyes), not the active drug. If you notice a change after switching, talk to your doctor. But don’t assume the generic is the problem.
Why don’t more biosimilars exist for popular biologics?
The main barrier isn’t science-it’s business. Brand-name companies use legal tactics, patent thickets, and pay-for-delay deals to block competition. Developing a biosimilar costs $100-200 million and takes 7-10 years. Many companies won’t invest if they think the market will be blocked. That’s why 90% of upcoming biologics have no biosimilar in development. Policy changes and public pressure are needed to break these patterns.
How do I know if my prescription is a generic?
Check the label. Generic drugs are listed by their chemical name, not the brand name. For example, instead of "Lipitor," you’ll see "atorvastatin." Your pharmacy receipt will also say "generic" or list the manufacturer. If you’re unsure, ask your pharmacist. They can tell you what you’re getting and how much you’re saving.


King Over
Generics work. I’ve been on them for years. No difference. Saved me $200 a month on blood pressure med. Simple as that.