Protein Medication Timing Calculator
Select Your Medication
When you take your morning pill with a bowl of scrambled eggs and a glass of milk, you might think you're doing the right thing-fueling your body before starting the day. But for people on certain medications, that breakfast could be quietly sabotaging their treatment. The truth is, protein-rich foods don’t just build muscle-they can block, delay, or reduce how well your medications work. This isn’t a myth. It’s science. And it’s happening more often than most people realize.
Why Protein Interferes with Medications
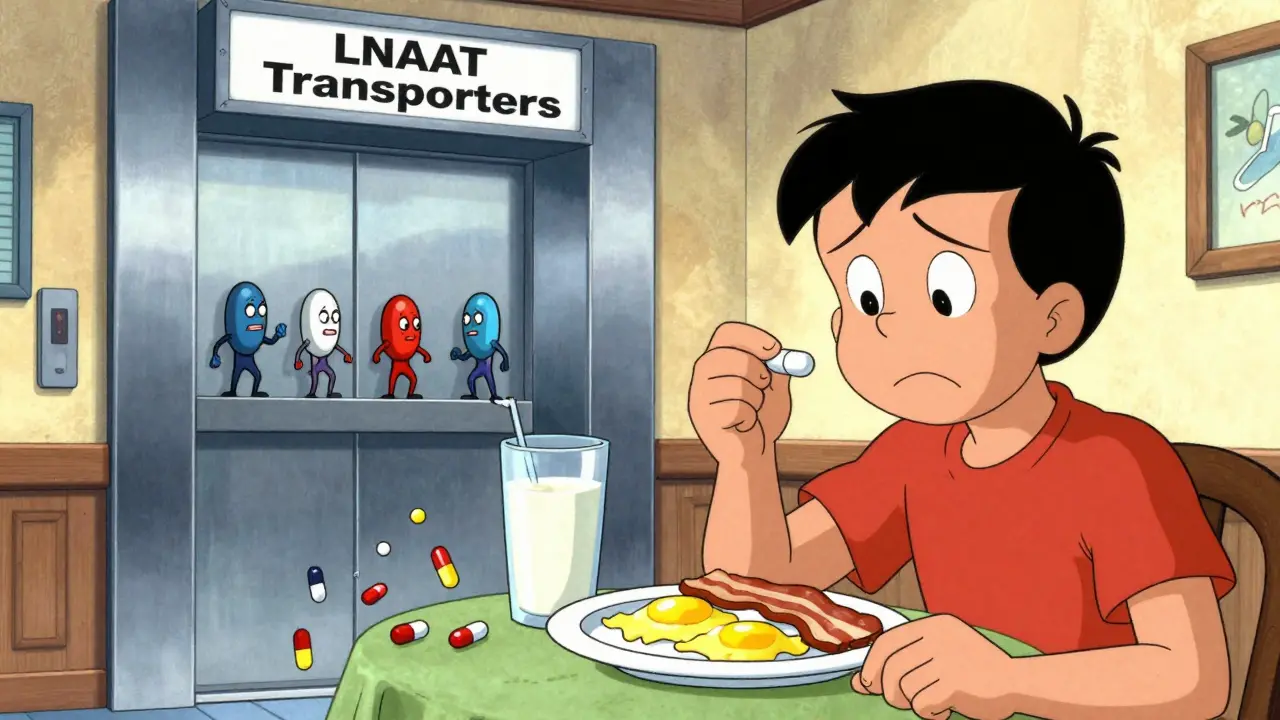
Protein doesn’t just sit in your stomach and wait to be digested. When you eat meat, fish, eggs, dairy, beans, or even a protein shake, your body breaks it down into amino acids. These amino acids flood your bloodstream, and your gut uses special transporters to move them into your system. The problem? Many medications use the exact same transporters. It’s like a crowded elevator-only so many people can get on at once. When amino acids are lining up, your medication gets pushed to the back. This is especially true for drugs that rely on large neutral amino acid transporters (LNAATs). Levodopa, the main treatment for Parkinson’s disease, is one of the most well-documented examples. Studies show that a high-protein meal can cut levodopa absorption by 30% to 50%. That means less of the drug reaches your brain, and your tremors, stiffness, or freezing episodes come back sooner. The same thing happens with some antibiotics, thyroid medications, and antiepileptic drugs like gabapentin and carbidopa. The Biopharmaceutics Classification System (BCS) helps explain why some drugs are more affected than others. Drugs in Class III-high solubility, low permeability-are the most vulnerable. Levodopa is one of them. It doesn’t dissolve poorly, but it struggles to cross the gut lining. Protein makes that crossing even harder. Meanwhile, drugs like ibuprofen or amoxicillin (Class I) aren’t as affected because they absorb easily regardless of what’s in your stomach.How Protein Changes Drug Timing
It’s not just about how much protein you eat-it’s when you eat it. High-protein meals slow down gastric emptying by 45 to 60 minutes. That means your pill sits in your stomach longer before moving into the small intestine, where most absorption happens. For drugs that need to hit the bloodstream fast, that delay can mean the difference between relief and a bad day. For levodopa users, the standard advice is to take the medication 30 to 60 minutes before eating. That gives it a head start. If you wait until after your meal, you’re competing with amino acids that are already racing through your gut. Some patients report that even a small protein snack-like a granola bar with 7 grams of protein-can trigger their symptoms to return within an hour. The Australian Prescriber review from 2024 confirmed that protein delays the time it takes for a drug to reach peak concentration (Tmax). That’s not just inconvenient-it can be dangerous. If you’re on a medication that needs to work quickly, like an antibiotic for an infection, waiting too long after eating could mean the drug doesn’t reach high enough levels to kill the bacteria.Not All Protein Is the Same
You might think, “I’ll just eat less protein.” But cutting protein too much can cause other problems. The Parkinson’s Foundation recommends 0.8 to 1.0 grams of protein per kilogram of body weight daily. For a 70kg person, that’s about 56 to 70 grams. If you drop below that, you risk muscle loss, weakness, and even malnutrition. A 2024 study in the Journal of Parkinson’s Disease found that 23% of patients on strict low-protein diets developed muscle wasting within 18 months. That’s why experts don’t recommend cutting protein overall-they recommend redistributing it. The protein redistribution diet works like this: eat only 30% of your daily protein at breakfast and lunch, and save 70% for dinner. This way, your daytime levodopa doses aren’t competing with protein, but your body still gets enough to repair tissue and maintain strength. People who’ve tried this report big changes. One Reddit user, u/ParkinsonsWarrior, tracked their symptoms with a wearable sensor and found their “off” time dropped from over five hours a day to just over two after switching to protein redistribution. That’s nearly three extra hours of mobility every single day.
What Other Medications Are Affected?
Levodopa is the poster child, but it’s not alone. Here’s a short list of medications that can be impacted by protein:- Levodopa/carbidopa - Absorption drops 25% with a 50g protein meal
- Penicillin antibiotics - Reduced absorption by 15-20% when taken with protein
- Carbidopa/levodopa extended-release - Less predictable absorption with meals
- Thyroid hormones (levothyroxine) - Protein can interfere with absorption, though fat and fiber play bigger roles
- Gabapentin and pregabalin - Use the same amino acid transporters as levodopa
- Alendronate (Fosamax) - Protein doesn’t directly interfere, but calcium-rich meals (often paired with protein) can block absorption
Real-Life Challenges
Knowing what to do is one thing. Doing it in real life is another. Dining out? Hard. A “healthy” salad might have grilled chicken, hard-boiled eggs, cheese, and nuts-adding up to 40 grams of protein before you even touch the bread. A protein shake labeled “low-sugar” might still have 20 grams of protein. Even a “high-fiber” oat bar can sneak in 5 grams or more. The Michael J. Fox Foundation’s 2024 survey of 1,243 patients found that 57% struggled with timing at first. But 78% improved after working with a dietitian who specialized in Parkinson’s. Many learned to use protein-modified foods-like bread with only 2 grams of protein instead of the usual 5-or to plan snacks with low-protein options: fruit, rice cakes, or plain crackers. Apps like “ProteinTracker for PD” help track intake. Users report 40% fewer timing mistakes. For people juggling multiple medications, daily routines, and changing symptoms, that kind of tool isn’t a luxury-it’s essential.
What Should You Do?
If you’re on a medication that might interact with protein, here’s what to do:- Check your prescription label. Look for warnings like “take on an empty stomach” or “avoid high-protein meals.”
- Ask your doctor or pharmacist. Don’t assume your med is safe. Many doctors don’t bring it up-68% of clinicians fail to discuss protein timing with new levodopa users, according to the American Society for Nutrition.
- Try timing your dose. Take your medication 30-60 minutes before meals. If nausea is an issue, have a low-protein snack (under 5g) like a banana or a few rice cakes.
- Consider protein redistribution. Save most of your protein for dinner. This is especially helpful for Parkinson’s patients.
- Use a food tracker. Apps can help you spot hidden protein in snacks, sauces, and “healthy” foods.

Adrienne Dagg
I can't believe people still don't get this 😤 I take my levodopa with a banana and water-no eggs, no yogurt, no 'healthy' protein shakes. If you're still eating a protein-packed breakfast and wondering why you're freezing up by 10 a.m., maybe stop blaming your meds and start blaming your toast with peanut butter. 🍌🚫🥜