RA Treatment Effectiveness Calculator
How this works: Select your current medications to see expected symptom improvement rates (ACR50/ACR70), side effect risks, and cost implications based on current medical research.
Your Medication Selection
Treatment Guidance
Key insight: The American College of Rheumatology guidelines recommend starting with methotrexate as the anchor drug. When combined with biologics, this approach shows significantly better results (50-60% ACR50 response) compared to biologics alone (30-40% ACR50).
Benefits of combination therapy
- 50-60% chance of achieving ACR50 response (50% symptom improvement)
- Higher likelihood of remission
- Reduced risk of joint damage progression
Potential risks
- Increased side effect risk with multiple medications
- Higher cost
- More frequent blood monitoring
When you're diagnosed with rheumatoid arthritis (RA), the goal isn't just to manage pain-it's to stop your immune system from tearing apart your joints. That’s where DMARDs come in. These aren’t regular painkillers. They’re disease-modifying drugs designed to slow or even halt the damage before it becomes permanent. But here’s the catch: not all DMARDs are the same. Some are old-school pills you swallow, others are injectable biologics that cost thousands a month. And when you mix them? The interactions can make or break your treatment.
What Exactly Are DMARDs and How Do They Work?
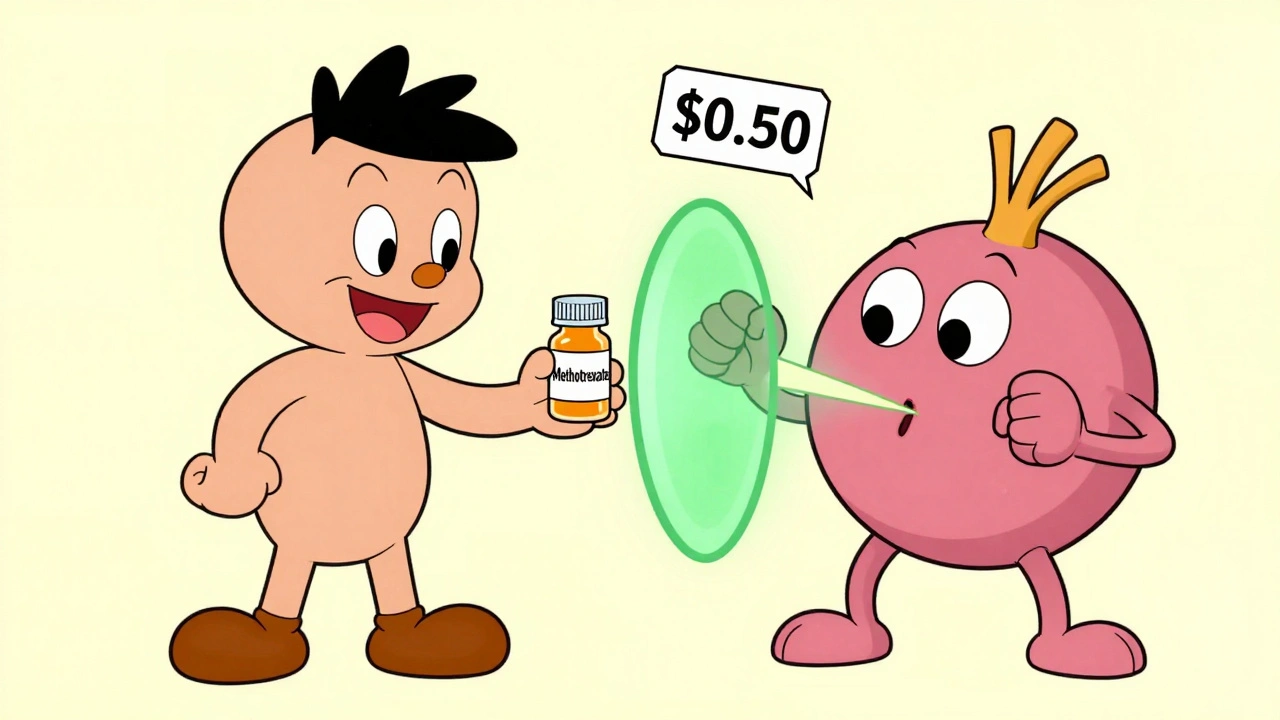
DMARD stands for disease-modifying antirheumatic drug. There are two main types: conventional synthetic DMARDs (csDMARDs) and biologic DMARDs (bDMARDs). The first group includes drugs like methotrexate, sulfasalazine, and hydroxychloroquine. Methotrexate, in particular, has been the backbone of RA treatment since the 1980s. It’s cheap-usually under $50 a month-and works by quietly shutting down overactive immune cells that attack your joints.
Biologics are different. They’re made from living cells, not chemicals. These are large protein molecules that zero in on specific parts of your immune system. For example, adalimumab and etanercept block TNF-alpha, a key inflammation signal. Rituximab wipes out B cells. Tocilizumab shuts down IL-6, another inflammation driver. These drugs don’t just calm things down-they redirect your immune system’s attack.
But there’s a trade-off. Biologics need to be injected or infused because your stomach would break them down if you swallowed them. You’ll need training to give yourself a shot. Some people get injection site reactions-redness, itching, swelling. Others dread the monthly IV clinic visits. Still, for many, the payoff is worth it: fewer flares, less joint damage, and better mobility.
Why Methotrexate Is Still the Anchor Drug
Even with all the fancy biologics on the market, methotrexate remains the first choice for most patients. Why? Because it works. In early RA, about 20-30% of people reach remission on methotrexate alone. That’s not bad for a pill that costs less than a daily coffee.
But here’s the real secret: methotrexate doesn’t just work by itself-it makes other drugs work better. Studies show that when you combine methotrexate with a biologic, the chance of hitting an ACR50 response (meaning at least 50% improvement in symptoms) jumps from 30-40% to 50-60%. That’s not a small boost. It’s the difference between still being disabled and getting back to work or playing with your kids.
Doctors call this combination therapy the gold standard. The 2021 American College of Rheumatology guidelines say: start with methotrexate. If you’re not improving after 3-6 months, add a biologic. Don’t skip straight to the expensive stuff unless you have severe disease, high antibody levels, or early joint damage.
Still, methotrexate isn’t easy for everyone. About 20-30% of patients can’t tolerate it. Nausea, fatigue, mouth sores-these are common. But there are fixes. Taking it at night, splitting the dose, or switching to a subcutaneous injection often helps. And folic acid (5-10 mg daily) cuts side effects by up to 70%. If methotrexate doesn’t stick, leflunomide or sulfasalazine can be alternatives.

Biologics: The High-Tech Option with High Costs
Biologics changed the game for RA. Before they existed, many people ended up in wheelchairs by their 40s. Now, with the right treatment, remission is possible. But they come with a price tag: $1,500 to $6,000 a month. That’s why biosimilars-cheaper copies of brand-name biologics-are now taking over. Adalimumab biosimilars like Amjevita and Cyltezo cost 15-30% less and work just as well.
Not all biologics are equal. Some, like anakinra, have weaker evidence and are rarely used anymore. Others, like rituximab, are reserved for patients who didn’t respond to TNF blockers. The choice depends on your antibodies, joint damage, and other health issues. For example, if you have heart disease, TNF inhibitors might be risky. If you’ve had tuberculosis, you can’t start a biologic without first being treated for it.
There’s also a newer class called JAK inhibitors-drugs like tofacitinib, baricitinib, and upadacitinib. These are pills, not injections. They block internal cell signals that trigger inflammation. In 2023, upadacitinib became the first JAK inhibitor approved as monotherapy for early RA. It matched methotrexate’s effectiveness in clinical trials. But they come with a black box warning: higher risk of serious infections, blood clots, and cancer. The FDA tightened labeling in 2021 after the ORAL Surveillance trial showed increased heart-related deaths in older patients.
Combination Therapy: When Two Are Better Than One
It’s not just methotrexate + biologic. Some patients get triple therapy: methotrexate + sulfasalazine + hydroxychloroquine. The CAMERA-II trial in 2013 found this combo worked just as well as methotrexate + adalimumab over two years. Same remission rates. Same joint protection. But triple therapy costs less than $300 a month.
So why don’t everyone use it? Because it’s not simple. Taking three pills daily is harder than one. Side effects stack up. And not all doctors are trained to manage this combo. Still, for patients without high-risk markers-like low RF or anti-CCP levels-this is a smart, affordable path.
On the flip side, if you have high disease activity, bone erosion on X-rays, or positive autoantibodies, biologics are the better bet. One study showed patients with these risk factors had a 40-50% chance of hitting ACR70 (70% symptom improvement) with a biologic combo-compared to just 25-35% with csDMARDs alone.

Real-World Challenges: Cost, Compliance, and Side Effects
Here’s the truth most clinics don’t talk about: people stop taking these drugs. A Swiss study found over a third of biologic users were on monotherapy-not because their doctor recommended it, but because they couldn’t tolerate methotrexate. Nausea, fatigue, or just plain frustration made them quit.
Cost is a huge barrier. In the U.S., 28% of RA patients skip doses because they can’t afford it. In India, biologics cost 300-500% of a monthly household income. That’s why so many there stick with csDMARDs.
Side effects are real. Infection is the biggest risk. About 19% of people on biologics report serious infections-pneumonia, urinary tract infections, even tuberculosis reactivation. That’s why everyone gets a TB skin test before starting. Some report injection site pain. Others get headaches or rashes. Rarely, there’s nerve damage or heart failure.
Still, patient satisfaction is high. In a 2022 survey of 1,247 RA patients, 78% said biologics improved their life. But 41% said cost was a major stressor. And on Reddit forums, people say they’d take the side effects if it meant they could walk without pain.
What’s Next? The Future of RA Treatment
The field is moving fast. In 2024, draft guidelines from the ACR now include ultrasound remission as a treatment goal-not just how you feel, but what the scan shows. That’s a big shift. It means doctors will be looking for invisible inflammation, not just joint swelling.
New drugs are coming too. Otilimab targets GM-CSF, a different inflammation pathway. Deucravacitinib is a more selective JAK inhibitor with fewer side effects. And researchers are testing drugs that reset immune cells entirely, not just suppress them.
But the biggest change might be accessibility. Biosimilars are expanding. Patient assistance programs now cover up to 50% of out-of-pocket costs. Specialty pharmacies handle delivery and education. You’re not alone in this.
RA treatment isn’t one-size-fits-all. It’s a puzzle. Your age, job, finances, side effect tolerance, and disease severity all matter. There’s no shame in starting with methotrexate. There’s no weakness in switching to a biologic when you need it. The goal isn’t to take the most drugs-it’s to take the right ones, at the right time, so you can live your life.
Can I take biologics without methotrexate?
Yes, but it’s usually less effective. Most biologics work better when combined with methotrexate. However, if you can’t tolerate methotrexate due to side effects like nausea or liver issues, your doctor may prescribe a biologic alone. Some JAK inhibitors, like upadacitinib, are approved for use without methotrexate in early RA. Still, combination therapy gives you the best shot at remission.
How long does it take for DMARDs and biologics to work?
Traditional DMARDs like methotrexate can take 6-12 weeks to show full effect. Biologics often work faster-some people notice improvement in 2-4 weeks, with maximum benefit around 12 weeks. JAK inhibitors are the quickest, sometimes working in as little as 2 weeks. Patience is key. These drugs don’t relieve pain like ibuprofen; they change the disease course over time.
Are biosimilars as good as brand-name biologics?
Yes. Biosimilars are not generics-they’re highly similar versions of the original biologic, made using the same living cells. The FDA requires them to show no meaningful difference in safety, purity, or potency. Studies show they work just as well for RA. Many patients switch without any change in symptoms. Biosimilars are now 15-30% cheaper, making treatment more affordable without sacrificing results.
Do I need blood tests while on DMARDs or biologics?
Yes, regularly. Methotrexate can affect your liver and blood counts, so you’ll need blood tests every 4-8 weeks. Biologics increase infection risk, so your doctor will monitor for signs of TB, hepatitis, and low white blood cells. JAK inhibitors require even stricter monitoring due to risks of blood clots and cancer. Skipping tests isn’t worth the risk. These drugs are powerful-your body needs watching.
What if my current medication stops working?
It’s common. RA is unpredictable. If your drug stops working, your rheumatologist won’t just increase the dose-they’ll likely switch you to a different class. For example, if a TNF inhibitor fails, you might try a B-cell blocker like rituximab or a JAK inhibitor. There are six classes of biologics and targeted DMARDs, so options exist. The key is catching the decline early-don’t wait until you’re in constant pain.
Can I drink alcohol while on methotrexate or biologics?
Limit it. Methotrexate can harm your liver, and alcohol adds to that risk. Most doctors recommend no more than one drink a week, if any. Biologics don’t directly interact with alcohol, but heavy drinking weakens your immune system, which increases infection risk-something you’re already more vulnerable to on these drugs. If you’re unsure, ask your doctor. Better safe than sorry.

patrick sui
Just read this and had to say: methotrexate + biologic is the real MVP combo. 🤝 I was on adalimumab alone for 6 months - barely moved the needle. Added methotrexate, and within 8 weeks, I could hold a coffee cup without wincing. Folic acid? Non-negotiable. Took mine with a glass of orange juice - tasted like a vitamin bomb but saved my stomach. 🍊