Clozapine Dose Adjustment Calculator
Current Dose & Status
Input your current clozapine dose and smoking status to see estimated blood levels.
Results
Therapeutic Range: 350-500 ng/mL
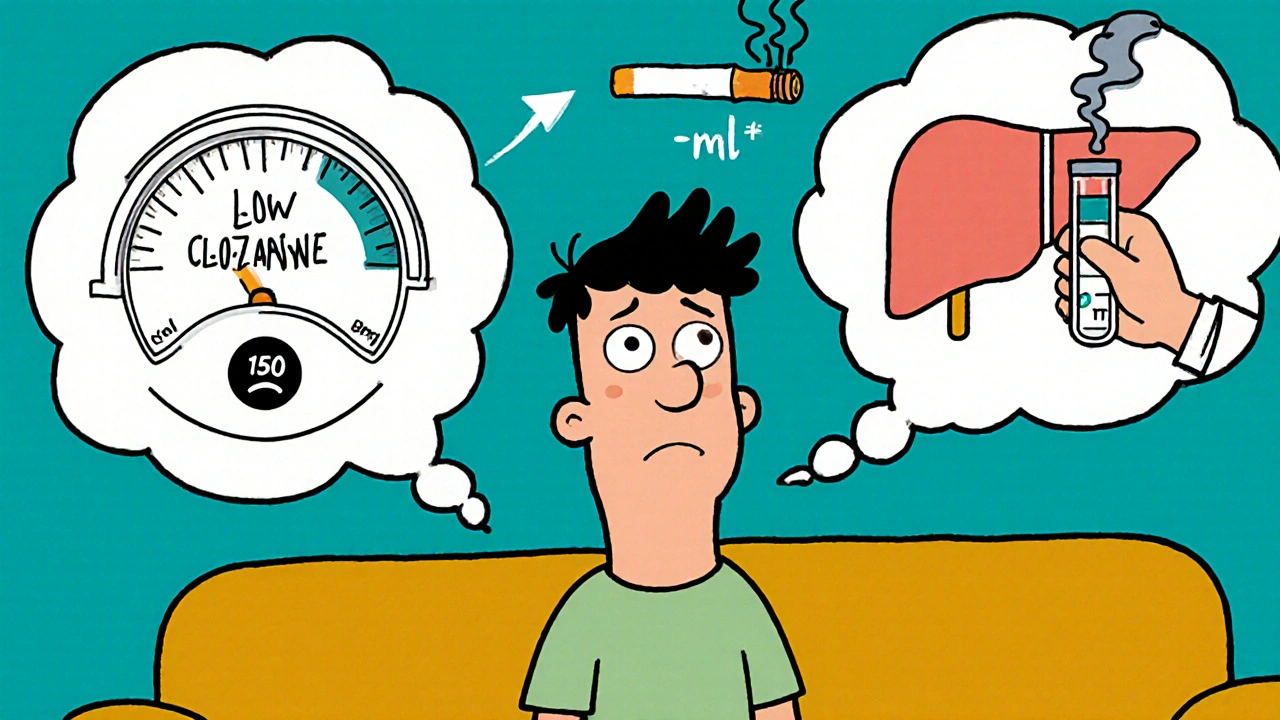
Why Smoking Can Make Your Clozapine Stop Working
If you’re taking clozapine for treatment-resistant schizophrenia, and you smoke cigarettes, your medication might not be working as well as you think. It’s not because you’re doing something wrong - it’s because your body is changing how it processes the drug. Tobacco smoke doesn’t just harm your lungs. It also turns up a key enzyme in your liver called CYP1A2, which breaks down clozapine faster than normal. This can drop your blood levels by 30% to 50%, leaving you vulnerable to relapse, hallucinations, or even hospitalization.
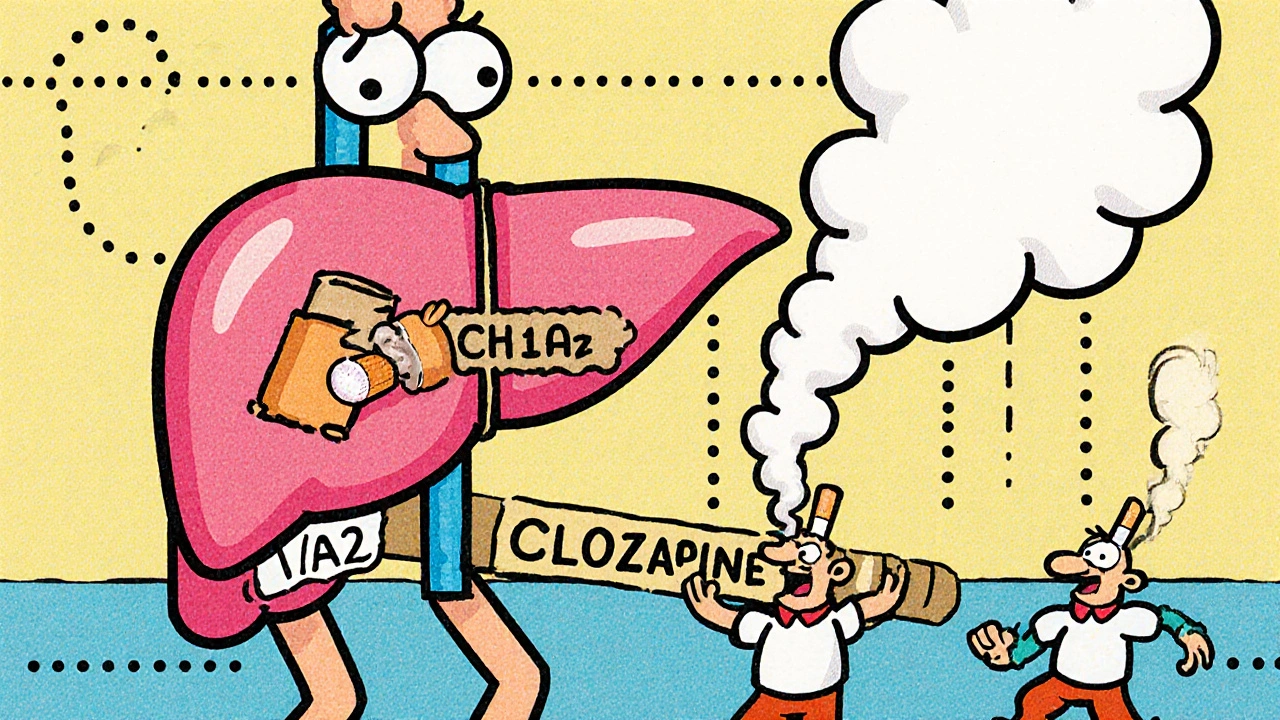
How CYP1A2 Turns Clozapine Into Nothing
Clozapine is broken down mainly by one enzyme: CYP1A2. This enzyme is like a factory worker that takes the drug apart into smaller pieces so your body can get rid of it. When you smoke, chemicals in tobacco - especially polycyclic aromatic hydrocarbons - bind to a receptor in your liver called AhR. This tells your liver to make more CYP1A2. More enzyme means faster breakdown. Within just two to three days of starting to smoke, your clozapine levels begin to fall. The effect sticks around for one to two weeks after you quit, which is why sudden smoking cessation can be dangerous.
Studies show that CYP1A2 handles 60-70% of clozapine clearance. That’s far more than other antipsychotics like olanzapine (30-40%) or risperidone (mostly handled by CYP2D6). This makes clozapine uniquely sensitive. A 2020 study in Nature confirmed that while lab tests once suggested CYP3A4 played a big role, real-world patient data shows CYP1A2 is the main player. And it’s not just cigarettes - e-cigarettes also trigger this effect, though slightly less strongly.
What Happens When You Start or Quit Smoking
Let’s say you’ve been stable on 300 mg of clozapine daily. Then you start smoking. Within a week, your blood levels drop from 400 ng/mL to 150 ng/mL - below the therapeutic range of 350-500 ng/mL. Your symptoms come back. You feel worse. Your doctor doesn’t know why - until they check your smoking status.
Now flip it: you quit smoking. Your CYP1A2 enzyme doesn’t shut off instantly. It takes days to slow down. But your dose hasn’t changed. So now, clozapine builds up in your system. Levels that were safe at 400 ng/mL might jump to 850 ng/mL. That’s toxic. You feel dizzy, your heart races, you’re overly sedated. In extreme cases, this can trigger seizures, heart inflammation, or even life-threatening drops in white blood cells.
Real cases back this up. One 32-year-old man was on 450 mg daily but still had subtherapeutic levels because he smoked heavily. His dose had to jump to 650 mg. Another woman quit smoking and stayed on her 400 mg dose. Within days, she was hospitalized with clozapine toxicity. Her dose was cut to 250 mg - and she stabilized.
Why Some People Are More Affected Than Others
Not everyone responds the same way. Genetics matter. People with the CYP1A2 *1F/*1F genotype have normal enzyme activity when not smoking - but when they light up, their enzyme activity spikes higher than average. This means they lose clozapine even faster. One 2024 case report in SAGE Open Medical Case Reports showed this group needed nearly double the dose of non-smokers to stay in range.
Other drugs can make this worse. Oxcarbazepine, used for seizures or mood disorders, is a strong CYP1A2 inducer too. If you’re on both, your clozapine levels can crash even without smoking. Alcohol? It’s a mild inhibitor - it might help temporarily, but it’s not safe or reliable. Coffee? It’s a weak CYP1A2 inhibitor, but not enough to counteract smoking.
What Doctors Should Do - And What You Should Ask For
Therapeutic drug monitoring isn’t optional for clozapine. It’s essential. Every time your smoking status changes - whether you start, stop, or cut back - your clozapine level must be checked. The American Psychiatric Association recommends checking levels 4-7 days after any dose change. If you’re starting to smoke, expect to increase your dose by 40-60%. If you quit, reduce it by 30-50%. Don’t guess. Test.
Many clinics now use electronic health record alerts. A 2023 JAMA Internal Medicine study showed these alerts cut adverse events by 37%. But not all systems have them. If your doctor doesn’t ask about smoking at every visit, ask them. Say: “My clozapine level hasn’t been checked since I started smoking. Can we test it?”
Psychiatrists surveyed on Doximity in 2023 reported that 68% check smoking status at every appointment. 82% adjust doses based on it. You deserve that level of care.

What If You Can’t Quit Smoking?
Quitting is hard - especially with schizophrenia. Nicotine can temporarily ease negative symptoms like apathy or social withdrawal. But the trade-off is dangerous. If quitting isn’t possible right now, don’t feel guilty. Work with your team to adjust your dose safely. There’s no shame in needing a higher dose to stay stable. Many patients report that once their dose was corrected, their symptoms improved for the first time in years.
Some patients have switched to other antipsychotics like quetiapine or aripiprazole to avoid this interaction. But clozapine is still the most effective drug for treatment-resistant cases. If you’ve tried others and failed, clozapine is worth holding onto - as long as you manage the smoking interaction properly.
The Bigger Picture: Why This Matters
Up to 70% of people on clozapine smoke - compared to 14% in the general U.S. population. That’s a massive gap. This interaction isn’t rare. It’s common. And it’s expensive. A 2021 study found unmanaged cases led to 22% higher hospitalization rates - costing about $14,500 per avoidable admission. The NIMH has poured $2.3 million into research on this exact issue.
Pharmacogenetic testing for CYP1A2 variants is growing. In 2018, only 15% of U.S. academic centers used it. By 2023, that jumped to 47%. Still, it’s not routine. But if you’ve had trouble with dosing, ask if genetic testing is an option. It could save you from years of trial and error.
New research is promising. A 2024 clinical trial is testing a sustained-release clozapine formulation designed to smooth out the spikes and drops caused by CYP1A2 induction. Early results show 40% less variability in blood levels among smokers. That could be a game-changer.
Bottom Line: Don’t Guess. Test.
Clozapine and tobacco smoke don’t mix safely - unless you’re monitoring closely. Smoking isn’t a moral failing. It’s a biological force that changes how your body handles medication. The solution isn’t to quit smoking before starting clozapine. It’s to know your smoking status, test your levels, and adjust your dose accordingly.
If you’re on clozapine and smoke - or used to smoke - ask your doctor for a blood level test. If they say it’s not necessary, ask again. Your stability, your safety, and your life depend on it.

Dolapo Eniola
Bro this is why I told my shrink to stop acting like I'm a criminal for smoking. CYP1A2 induction isn't a choice, it's biology. My dose went from 300 to 600mg in 3 weeks and they still acted like I was cheating the system. 😤