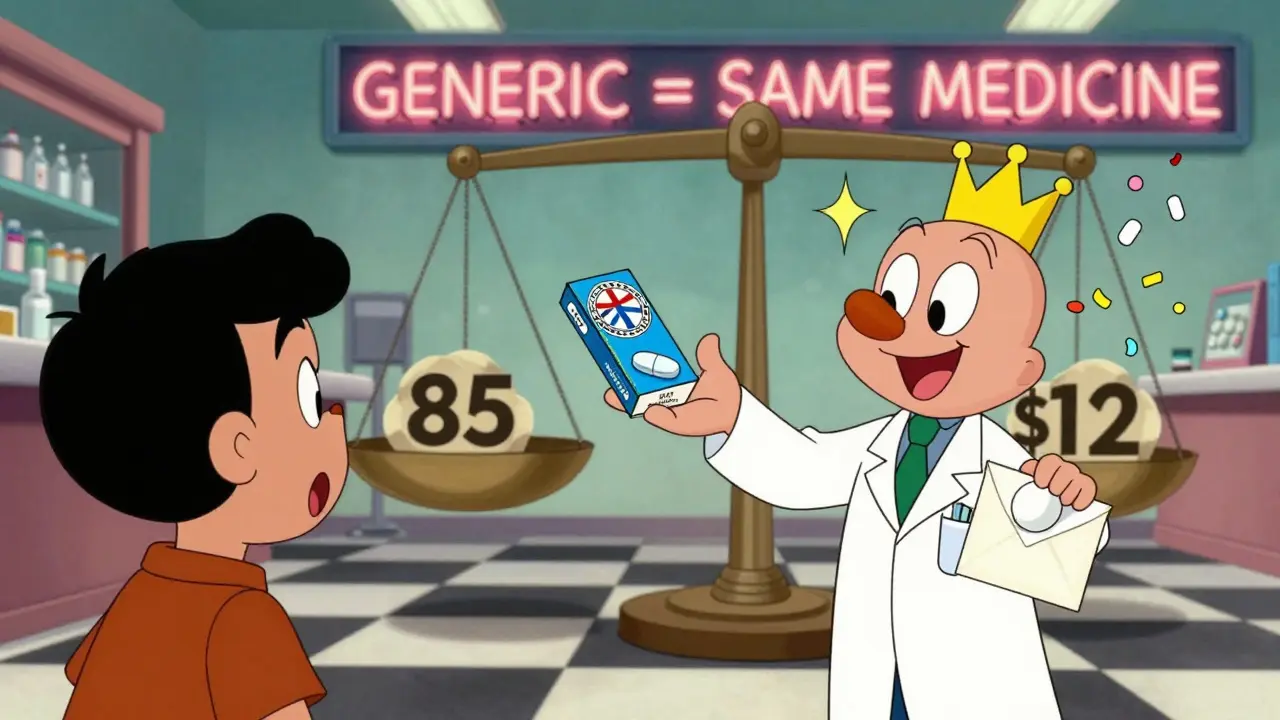
Let’s say you’re handed a prescription for a common medication-maybe something like lisinopril for blood pressure or atorvastatin for cholesterol. The pharmacist hands you two options: the familiar blue pill in the branded box, or a plain white pill with a simple label. The brand costs $85. The generic? $12. You pause. Is the cheaper one really the same? Should you risk it?
The truth is, you’re not alone in wondering. Millions of people in the U.S. face this choice every month. And the answer isn’t about luck or guesswork. It’s about science, regulation, and market forces that have quietly transformed how we pay for medicine.
What Exactly Is a Generic Drug?
A generic drug isn’t a copy. It’s not a knockoff. It’s the exact same medicine as the brand-name version, down to the active ingredient. That means if your brand-name drug contains 20 mg of atorvastatin, the generic has 20 mg of atorvastatin-nothing more, nothing less. The FDA requires that generics match the brand in strength, dosage form, route of administration, and how quickly the body absorbs it.
The key difference? The inactive ingredients. The color, shape, flavor, or filler materials might be different. But those don’t affect how the drug works. Think of it like two identical cars-one with a shiny logo, the other without. Same engine. Same fuel efficiency. Same safety rating. Just a different sticker.
The legal pathway for generics was created in 1984 by the Hatch-Waxman Act. Before that, every new version of a drug had to go through full clinical trials-costing hundreds of millions. The law changed that. Generics only need to prove they’re bioequivalent: meaning they deliver the same amount of active ingredient into your bloodstream at the same rate as the brand. The FDA allows a tiny margin-80% to 125%-for absorption differences. That’s not a loophole. It’s a scientifically accepted range that still ensures the same therapeutic effect.
How Much Cheaper Are Generics Really?
The numbers don’t lie. As of 2024, generic drugs made up 90% of all prescriptions filled in the U.S. But they accounted for just 12% of total spending on prescriptions. That’s the power of scale and competition.
On average, generics cost 79% to 85% less than their brand-name equivalents. For example:
- Lisinopril (brand: Prinivil, Zestril) - Brand: $120/month. Generic: $4/month.
- Atorvastatin (brand: Lipitor) - Brand: $200/month. Generic: $10/month.
- Omeprazole (brand: Prilosec) - Brand: $150/month. Generic: $8/month.
These aren’t outliers. This is the norm. The U.S. Department of Health and Human Services found that after just three years of generic competition, prices typically fall to 20% of what they were before. With five or more generic manufacturers, prices often drop below half the original brand price.
And here’s the twist: brand-name drug companies aren’t just sitting still. When generics enter the market, many brands cut their own prices to stay competitive. In 2025, Bayer lowered the list price of Nexavar by 50% after its first generic launched. Merck dropped Januvia’s price by over 42%. Why? Because they know the market is shifting-and they’re trying to hold onto patients before Medicare’s new price caps kick in.
Why Do Brand Drugs Cost So Much?
It’s not because they’re better. It’s because they’re protected.
Brand-name companies spend years and billions developing a drug. They get a patent that gives them exclusive rights to sell it-usually for 20 years. During that time, they set high prices to recoup R&D costs and make a profit. That’s the deal: innovation is funded by high prices.
But once the patent expires, anyone can make the drug. And when multiple companies start making it, prices collapse. That’s the free market at work. One generic? Price drops to about 90% of the brand. Three or four? Down to 60-70%. Five or more? Often below 50%.
The U.S. system is unique. While other countries cap drug prices directly, the U.S. lets the market decide. The result? Brand drugs here are among the most expensive in the world. But generics? They’re the cheapest. That’s why, despite the high list prices of brand-name drugs, the U.S. actually spends 18% less per prescription on average than Canada, Germany, or the UK-because 9 out of every 10 prescriptions are filled with generics.

Do Generics Work the Same?
Yes. And the evidence is overwhelming.
The FDA doesn’t approve generics lightly. They require the same quality controls, manufacturing standards, and stability testing as brand-name drugs. Every batch is inspected. Every facility is audited. Generics aren’t made in basement labs. Most are made in the same factories as the brand, just under a different label.
A 2025 survey of over 1,000 Americans found that 84% believe generics are just as effective as brand-name drugs. But here’s the disconnect: 62% still trust the brand more. Why? Because of marketing. Because of the logo. Because of the fear that “if it looks different, it must be different.”
Real-world studies back up the science. A major analysis by the American Medical Association reviewed more than 50 clinical trials comparing generics and brands. Not one showed a meaningful difference in effectiveness or safety. The same goes for studies from the National Academy of Medicine and the Cochrane Collaboration.
Doctors know this. That’s why most prescribe generics by default. If you’re on a brand drug and your doctor says, “Let’s switch to the generic,” they’re not cutting corners. They’re saving you money without sacrificing care.
Why Do Some People Still Choose Brands?
Cost isn’t the only factor. Perception matters.
Many people stick with brands because they’ve been using them for years. They remember the brand name from TV ads. They trust the name they know. Some worry that switching will cause side effects-even though there’s no scientific reason it should.
There’s also the placebo effect. If you believe the brand works better, you might feel better on it-even if the drug is identical. That’s real. But it’s not the drug working differently. It’s your mind.
Another reason? Insurance. Some plans make it harder to get generics. Maybe they require prior authorization. Or they charge a higher copay for the generic. That’s rare, but it happens. Always check your plan’s formulary. Most insurers push generics because they save money-and they pass those savings to you.
And then there’s the rare case where a generic might not work for you. It’s uncommon, but possible. Some people are sensitive to the inactive ingredients. Maybe the filler causes stomach upset. Or the pill size is too big to swallow. In those cases, switching back to the brand is fine. But don’t assume it’s the active ingredient. Talk to your pharmacist. They can help you find a generic with a different filler or formulation.
What’s Changing in 2025 and Beyond?
The game is shifting fast.
The Inflation Reduction Act, which takes full effect in January 2026, will cap insulin at $35 per month and set a $2,000 annual out-of-pocket cap for Medicare Part D users. That means even if you’re on a brand drug, your costs will be limited. But here’s the catch: the law also allows Medicare to negotiate prices for 10 high-cost brand drugs each year starting in 2026. That will push more brands to lower their prices-or lose Medicare coverage entirely.
At the same time, more biosimilars (generic versions of complex biologic drugs) are hitting the market. These used to cost tens of thousands per year. Now, they’re coming in at 60-70% less. Drugs for arthritis, cancer, and autoimmune diseases are seeing big drops.
And the trend is clear: the more generics enter the market, the more brand-name companies cut prices. The cycle keeps going. The result? Lower costs across the board.
What Should You Do?
Here’s your simple action plan:
- Ask your doctor: “Is there a generic version of this drug?”
- Ask your pharmacist: “What’s the cash price for the generic?” Sometimes it’s cheaper than your insurance copay.
- Check your plan’s formulary. If the generic is preferred, you’ll pay less.
- If you’ve had trouble with a generic before, tell your provider. There might be another option.
- Don’t assume brand = better. It usually just means more marketing.
Every time you choose a generic, you’re not just saving money. You’re helping lower healthcare costs for everyone. Generics are the only part of the U.S. drug system that consistently reduces overall spending. Since 2019, Americans have saved over $6.4 billion just by using generics-even as more of them were prescribed.
The bottom line? Generics are safe. They’re effective. And they’re dramatically cheaper. There’s no reason not to use them-unless your doctor says otherwise. And even then, it’s worth asking why.
Frequently Asked Questions
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for quality, strength, purity, and stability as brand-name drugs. They’re made in the same types of facilities and undergo the same inspections. There’s no evidence that generics are less safe.
Why do generics look different from brand drugs?
By law, generics can’t look exactly like the brand drug, even if they contain the same active ingredient. That’s to avoid confusion and trademark issues. The color, shape, or flavor may be different-but the medicine inside works the same way.
Can I switch from a brand drug to a generic without problems?
For most people, yes. Thousands of studies show no difference in effectiveness or side effects. If you’ve been on a brand drug for years and your doctor recommends switching, it’s safe. If you’re worried, start with a small change-like switching one prescription at a time-and monitor how you feel.
Why are some generic drugs more expensive than others?
It depends on competition. If only one company makes the generic, it might cost more. If five or six companies make it, prices drop sharply. Also, some generics are made overseas and have higher shipping or regulatory costs. Always compare prices at different pharmacies.
Do insurance plans cover generics better than brands?
Yes. Most insurance plans put generics in the lowest cost tier. That means lower copays. Sometimes, the cash price of a generic is cheaper than your insurance copay for the brand. Always ask your pharmacist to check both options.

SWAPNIL SIDAM
Wow. This is the first time I read something about medicine that actually made sense. In India, we take generics every day-no choice, really. But seeing it explained like this? It’s like someone finally turned on the light in a dark room.