What Are Immune-Related Adverse Events (irAEs)?
When your immune system fights cancer, it can sometimes turn on your own body. This is the reality behind immune-related adverse events, or irAEs. These are side effects caused by immune checkpoint inhibitors (ICIs)-drugs like pembrolizumab, nivolumab, and ipilimumab-that help the immune system recognize and attack cancer cells. But in doing so, they can also trigger inflammation or autoimmune reactions in healthy tissues. irAEs aren’t rare. About 83% of patients on CTLA-4 inhibitors, 72% on PD-1 inhibitors, and 60% on PD-L1 inhibitors will experience at least one. They can show up weeks or even months after treatment starts-or after it ends.
Which Organs Are Most Affected?
Not all irAEs are the same. Some are common. Others are rare but dangerous. The most frequent involve the skin, gut, and endocrine system. Skin rashes, itching, and blistering happen in up to 40% of patients. Diarrhea and colitis show up in 20-30%, and thyroid problems like hypothyroidism occur in 10-20%. These are often manageable. But less common irAEs can be life-threatening. Myocarditis (heart inflammation) affects less than 1% of patients, but has a 2.7% fatality rate. Pneumonitis (lung inflammation) and neurological issues like meningitis or neuropathy are rare but need urgent care. Hepatitis (liver inflammation) and kidney damage also occur. The key is knowing which symptoms to watch for-and acting fast.
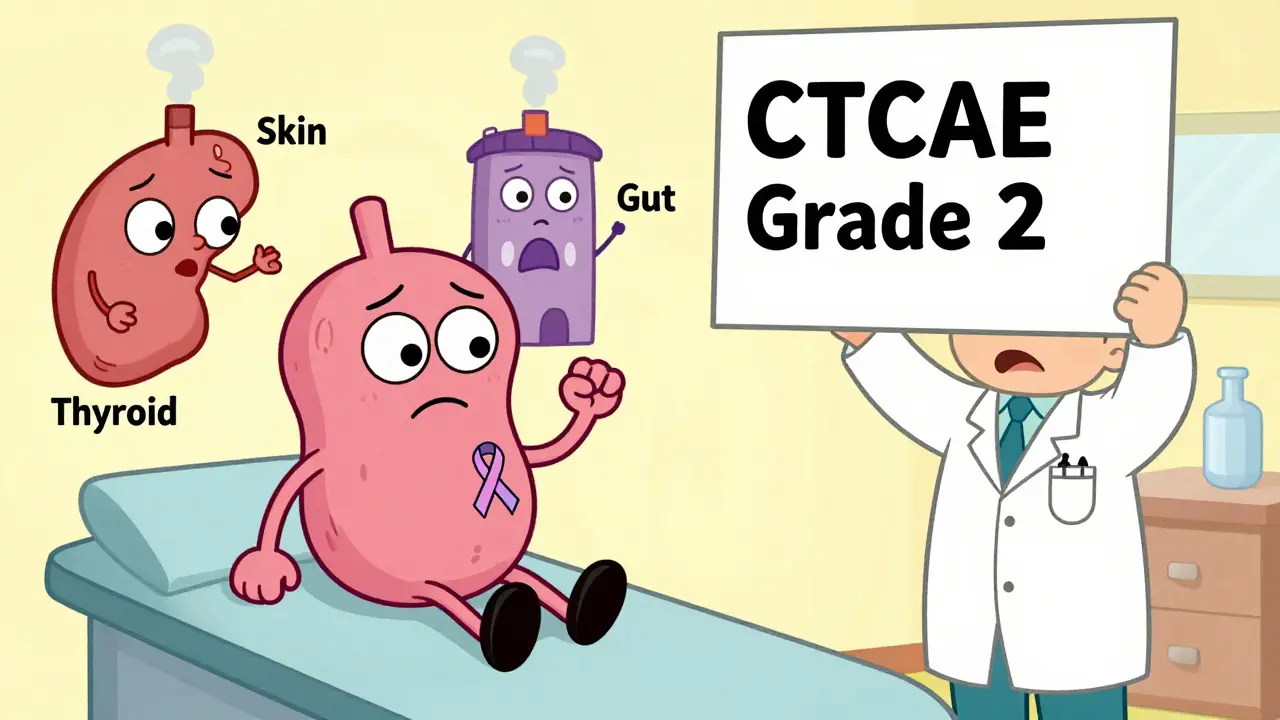
How Are irAEs Graded and Diagnosed?
Doctors use the Common Terminology Criteria for Adverse Events (CTCAE) to rate irAEs from Grade 1 to Grade 4. Grade 1 means mild symptoms that don’t interfere with daily life-like a small rash or slight fatigue. Grade 2 is moderate-enough to disrupt normal activities, like diarrhea more than 4 times a day or fatigue that limits work. Grade 3 is severe: hospitalization may be needed. Grade 4 is life-threatening. The first step in diagnosing an irAE is ruling out other causes. Is that diarrhea from an infection? Is that cough from pneumonia? Blood tests, imaging, and sometimes biopsies are needed. You can’t assume it’s an irAE without checking. That’s why oncology teams now require labs and specialist input before starting treatment.
What’s the First Line of Treatment?
Corticosteroids are the cornerstone of irAE management. For Grade 2 irAEs, doctors typically start oral prednisolone at 1 mg per kg of body weight per day. For Grade 3 or 4, intravenous methylprednisolone at 1-2 mg/kg/day (up to 1 gram daily) is given for at least 3 days, then switched to high-dose oral steroids. The goal isn’t just to suppress symptoms-it’s to stop the immune system from attacking your organs. Treatment pauses the cancer therapy until symptoms improve to Grade 1 or lower. Then, steroids are slowly tapered over 4 to 6 weeks. Rushing this step can cause rebound inflammation. Many patients don’t realize how long this process takes. One study found 68% of patients struggled with steroid side effects like weight gain, insomnia, and mood swings during tapering.

What If Steroids Don’t Work?
Not all irAEs respond to steroids. When symptoms don’t improve after 48 hours, it’s called steroid-refractory. At that point, doctors turn to stronger immunosuppressants. Infliximab, a drug that blocks TNF-alpha, is often used for colitis or hepatitis. Mycophenolate mofetil works for lung or liver issues. IVIG (intravenous immune globulin) is used for neurological or blood-related irAEs. Cyclophosphamide is reserved for the most severe cases. Newer options are emerging. Vedolizumab, originally for Crohn’s disease, is now showing strong results in steroid-refractory colitis-with a 68% response rate compared to 52% for infliximab, according to SITC’s 2024 guidelines. Clinical trials like NCT04438382 and NCT04407247 are comparing these drugs head-to-head to find the best fit for each organ.
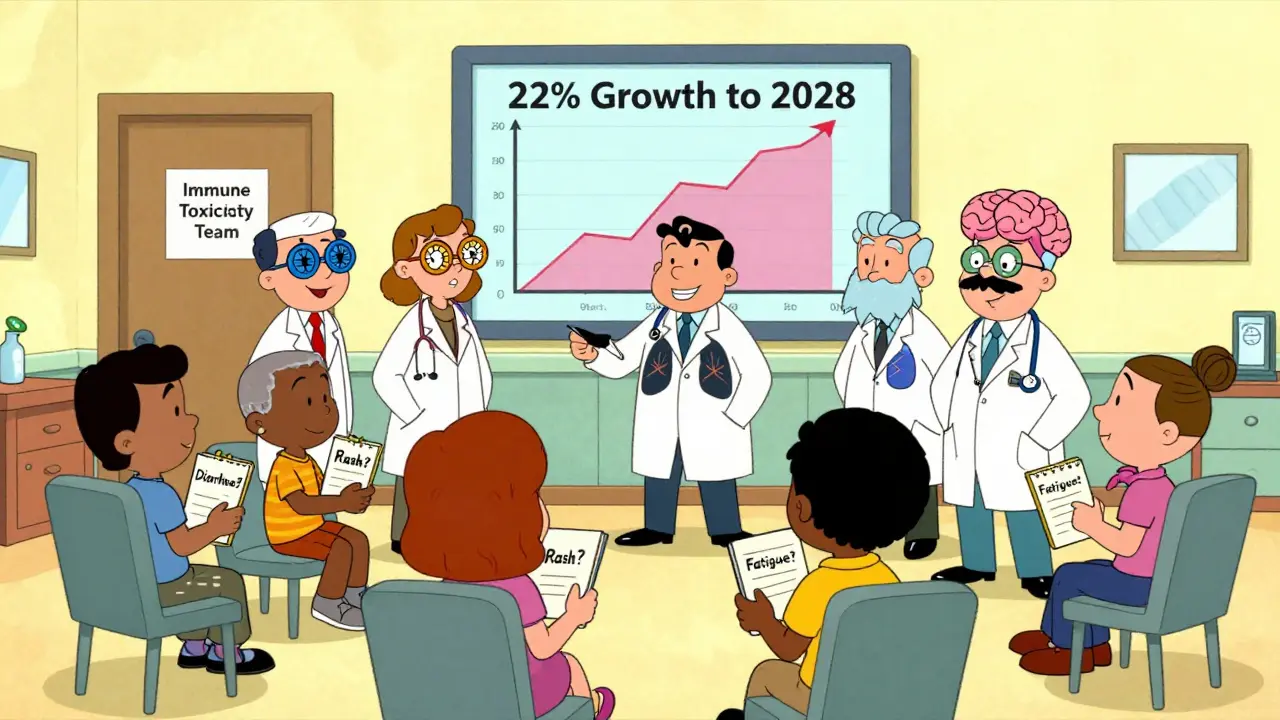
Why Timing and Specialist Involvement Matter
irAEs don’t wait. Delayed treatment can mean permanent damage-or death. A 2023 Flatiron Health analysis of over 12,500 patients showed that starting treatment within 48 hours of symptom onset cut hospitalization rates from 34% to 19%. That’s why leading cancer centers now have dedicated immune toxicity teams. These teams include oncologists, endocrinologists, gastroenterologists, pulmonologists, and neurologists-all on standby. For Grade 3 or 4 events, specialist consultation must happen within 24 hours. Community clinics without these resources struggle. A 2022 study found that those with formal protocols reduced severe complications by 37%. Hospitals using Epic’s 2023 oncology update now get automated alerts when patients report symptoms like diarrhea or shortness of breath, triggering immediate referrals.
Can You Still Beat Cancer While Managing irAEs?
One big fear among patients: will treating irAEs make the cancer come back? The answer is no. Multiple studies, including a 2022 review in Cancer Therapy Advisor, confirm that immunosuppressive therapy for irAEs doesn’t reduce the effectiveness of immune checkpoint inhibitors. Patients who needed infliximab or steroids for colitis still had the same tumor response rates as those who didn’t. This is critical. You don’t have to choose between survival and side effects. The goal is to control the immune reaction without shutting down the anti-cancer response. That balance is why expert protocols exist.
What About Long-Term Effects?
Most irAEs resolve with treatment. About 85-90% of cases are fully reversible. But 10-15% become chronic. Thyroid damage often means lifelong hormone replacement. Some patients need ongoing low-dose steroids or immunosuppressants. Others develop permanent nerve damage or lung scarring. That’s why follow-up doesn’t end when treatment does. Patients need annual blood work, imaging, and specialist check-ups-even years after stopping ICIs. A 2023 patient survey in The Oncologist found that 41% didn’t understand they might need lifelong care for irAEs. Education gaps like this are dangerous.
What’s Changing in irAE Management?
The field is moving fast. Researchers are now looking for biomarkers that predict who’s at risk. A 2023 Nature Medicine study found that patients with baseline IL-17 levels above 5.2 pg/mL had nearly five times the risk of severe irAEs. That could lead to pre-treatment screening. ESMO is rolling out patient education materials in 15 languages to fix communication gaps. Epic’s automated alerts are becoming standard. And with over 287 ICI combinations now in trials, irAEs will only become more common. Specialized irAE clinics are projected to grow 22% annually through 2028. The future isn’t just about treating side effects-it’s about preventing them before they start.
What Should Patients Do?
If you’re on an immune checkpoint inhibitor, know the warning signs: persistent diarrhea, unexplained fatigue, rash that spreads, shortness of breath, chest pain, new headaches, vision changes, or muscle weakness. Don’t wait. Call your oncology team immediately-even if it’s late at night. Keep a symptom journal. Track when things started, how bad they are, and what makes them better or worse. Ask for a copy of your irAE management plan. Understand your steroid taper schedule. Know who to call after hours. Most importantly: don’t ignore symptoms because you’re afraid of stopping cancer treatment. Managing irAEs isn’t a setback-it’s part of staying alive.

Joie Cregin
I just started my third round of pembrolizumab last month, and honestly? This post felt like someone reached into my brain and wrote down every fear and win I’ve had. That bit about the steroid taper? Yeah. I cried reading that. 68% struggle with side effects? Me too. But I’m still here. Still fighting. And I’m not alone.