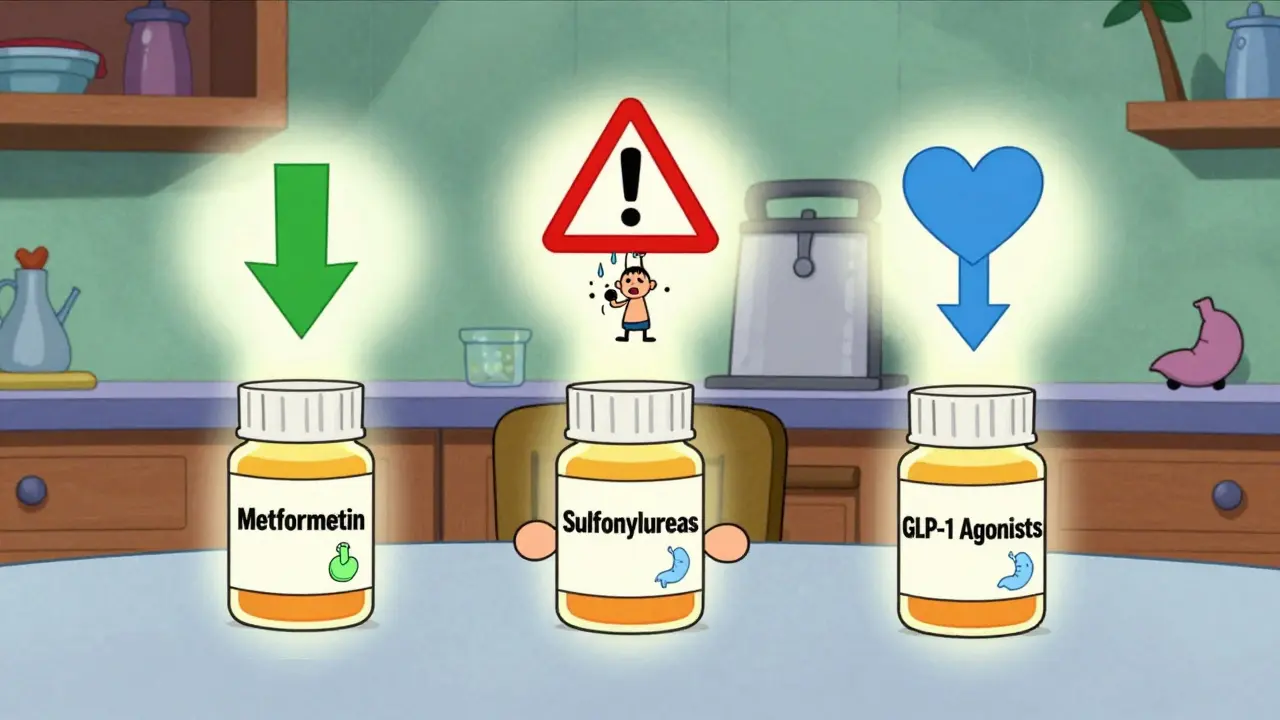
When you're managing type 2 diabetes, choosing the right medication isn't just about lowering blood sugar-it's about what works for your body, lifestyle, and long-term health. Three oral medications dominate the conversation: metformin, sulfonylureas, and GLP-1 receptor agonists. Each has different strengths, side effects, and risks. And while they all aim to control blood glucose, they do it in completely different ways.
Metformin: The Longtime Standard
Metformin has been the go-to first-line treatment for type 2 diabetes for over two decades. It's cheap, widely available as a generic, and has decades of safety data behind it. The drug works by reducing how much sugar your liver releases into your bloodstream and by helping your muscles use insulin more effectively. It doesn’t force your pancreas to make more insulin-it just helps your body use what it already has.
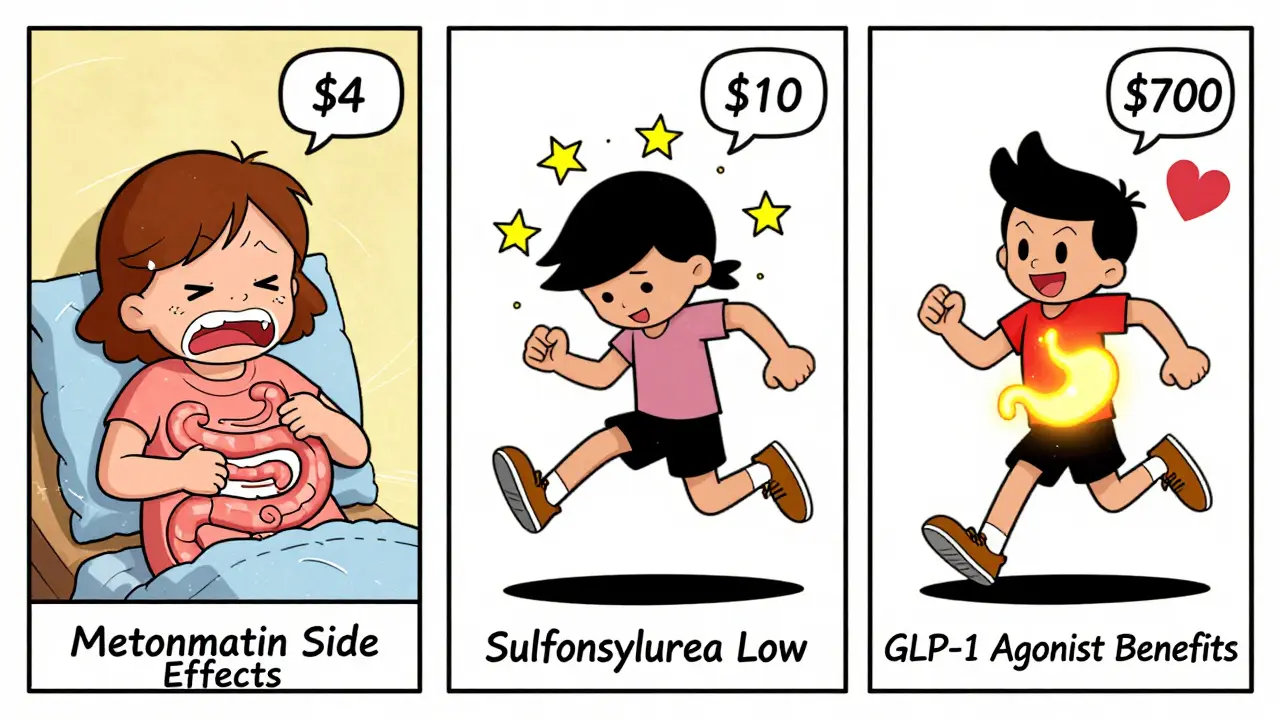
Most people take it twice a day with meals to reduce stomach upset. Extended-release versions are now common, easing side effects like nausea and diarrhea, which affect 20-30% of users at first. For many, these symptoms fade after a few weeks. If you can tolerate it, metformin typically lowers HbA1c by 1.0-2.0%. That’s a solid drop, especially considering it doesn’t cause weight gain. In fact, many people lose 2-3 kg over time.
It’s not perfect. Some people just can’t handle the gastrointestinal side effects, no matter the formulation. One patient in Perth told me they tried every brand and dose-immediate release, extended release, even splitting doses-and still had constant diarrhea. For those people, metformin isn’t an option.
Another thing to know: metformin requires healthy kidneys. If your eGFR drops below 45 mL/min/1.73m², your doctor will likely reduce your dose or stop it altogether. There’s a rare but serious risk of lactic acidosis if you have severe kidney disease, heart failure, or drink heavily. That’s why doctors check kidney function before starting and every year after.
Sulfonylureas: The Old Workhorse with Hidden Costs
Sulfonylureas like glimepiride (Amaryl) and glipizide (Glucotrol) were the first oral diabetes drugs ever developed-in the 1950s. They work by telling your pancreas to pump out more insulin, no matter what your blood sugar level is. That’s powerful-but also dangerous.
They can lower HbA1c by 1.0-1.5%, which sounds good. But here’s the catch: because they force insulin out regardless of your blood sugar, they cause hypoglycemia. About 15-30% of people on sulfonylureas have mild to moderate low blood sugar episodes each year. For 2-4%, it’s severe enough to require emergency help. That means confusion, shaking, sweating, passing out-even seizures. And because these episodes can happen at night or without warning, they’re hard to predict.
Weight gain is another issue. Most people gain 2-4 kg on sulfonylureas. That’s the opposite of what most people with type 2 diabetes need. And unlike metformin or newer drugs, sulfonylureas don’t protect your heart. Some studies even suggest they might slightly increase cardiovascular risk compared to other options.
They’re still used, especially where cost is a concern. Generic glipizide can cost as little as $10 a month. But for many patients, the trade-offs aren’t worth it. One patient on HealthUnlocked described four ER visits in three years because of low blood sugar while on glipizide. After switching to a different medication, her blood sugars stabilized. She didn’t mention weight loss-just safety.
GLP-1 Agonists: The New Powerhouse
GLP-1 receptor agonists changed the game. Originally developed as injectables like liraglutide (Victoza) and semaglutide (Ozempic), they’re now available as an oral pill-rybelsus. These drugs mimic a natural hormone your gut releases after eating. It slows digestion, tells your pancreas to release insulin only when blood sugar is high, and signals your brain to feel full.
The results? HbA1c drops by 0.8-1.5%, but the real wins are weight loss and heart protection. Most people lose 3-6 kg, sometimes more. In clinical trials, semaglutide users lost up to 18 pounds without changing their diet. And unlike sulfonylureas, GLP-1 agonists rarely cause low blood sugar-unless you’re also taking insulin.
They also reduce heart attacks, strokes, and heart failure. The LEADER trial showed liraglutide cut major cardiovascular events by 13%. That’s why the American Diabetes Association now recommends GLP-1 agonists as second-line therapy for anyone with heart disease, kidney disease, or high cardiovascular risk-even if their HbA1c isn’t that high.
But they’re not easy. Nausea, vomiting, and diarrhea hit 20-40% of users, especially at first. Dose escalation is slow: every four weeks, to give your stomach time to adjust. Still, many patients say the trade-off is worth it. One person on the ADA forums shared: "I had 18 pounds off in three months. My A1C went from 7.8 to 6.2. The nausea was rough, but I pushed through. Best decision I ever made."
Cost is the biggest barrier. Injectable versions can run $700-$900 a month without insurance. Oral semaglutide (Rybelsus) is slightly cheaper but still costs $500-$700. That’s why many people stick with metformin or sulfonylureas-even if they’re less effective. Some manufacturers offer copay cards that bring it down to $0, but eligibility is strict.

How They Compare Side by Side
| Feature | Metformin | Sulfonylureas | GLP-1 Agonists |
|---|---|---|---|
| HbA1c Reduction | 1.0-2.0% | 1.0-1.5% | 0.8-1.5% |
| Weight Effect | Neutral or loss (2-3 kg) | Gain (2-4 kg) | Loss (3-6 kg) |
| Hypoglycemia Risk | Very low | High (15-30% yearly) | Low (unless with insulin) |
| Cardiovascular Benefit | Mildly protective | Neutral or slightly negative | Strongly protective |
| Common Side Effects | Diarrhea, nausea | Hypoglycemia, weight gain | Nausea, vomiting, diarrhea |
| Cost (Monthly, US) | $4-$10 (generic) | $10-$30 (generic) | $500-$900 |
| Administration | Oral, 1-2x/day | Oral, 1-2x/day | Oral (Rybelsus) or injectable |
| Renal Limitations | eGFR ≥45 for full dose | eGFR ≥30 | Minimal restrictions |
What Experts Say and What Patients Experience
Doctors are shifting their approach. The 2022 ADA guidelines say metformin is still first-line-but GLP-1 agonists should be considered early for people with heart disease or obesity. Sulfonylureas? They’re becoming a last resort.
Real-world data backs this up. In 2023, semaglutide (Ozempic) became the third most prescribed diabetes drug in the U.S., with over 12 million prescriptions. Sulfonylureas dropped to 8.2 million. More patients are switching from sulfonylureas to GLP-1 agonists than ever before.
But patient experiences are mixed. One Reddit user wrote: "Metformin gives me constant diarrhea. I’ve tried everything. I’m on GLP-1 now and the nausea is awful, but at least I’m not crashing from low blood sugar anymore." Another said: "I switched from Ozempic to glipizide because I couldn’t afford it. My sugar went up, and I gained 10 pounds. I’d rather be sick than broke."
Cost isn’t just a footnote-it’s a dealbreaker. In Australia, GLP-1 agonists aren’t fully subsidized. Many patients pay hundreds out of pocket. That’s why some doctors still start with metformin, then move to sulfonylureas if needed, before considering GLP-1 agonists.
What You Should Ask Your Doctor
If you’re starting or switching medications, here’s what to bring up:
- "Do I have heart disease, kidney disease, or high risk for either?" (If yes, GLP-1 agonists may be best.)
- "Can I handle nausea or diarrhea if they happen?" (GLP-1 agonists require tolerance.)
- "Am I at risk for low blood sugar?" (If you drive, work nights, or have unpredictable meals, avoid sulfonylureas.)
- "What’s my kidney function?" (Critical for metformin and sulfonylureas.)
- "What’s my out-of-pocket cost?" (Metformin is $10. GLP-1 agonists can be $800. That matters.)
There’s no one-size-fits-all. The best drug is the one you can take safely, affordably, and consistently. For some, that’s metformin. For others, it’s GLP-1 agonists. For a few, sulfonylureas are the only option left.
What’s Next?
The future is moving fast. Oral GLP-1 agonists like Rybelsus are making adherence easier. New triple agonists (targeting GLP-1, GIP, and glucagon) are in trials and showing HbA1c drops of over 3% and weight loss of nearly 25%. These could become first-line in five years.
But until then, the choice comes down to balance: effectiveness, safety, cost, and tolerability. Don’t assume the newest drug is right for you. Don’t assume the cheapest is safe. Talk to your doctor. Track your symptoms. And remember: your treatment should fit your life-not the other way around.
Is metformin still the best first choice for type 2 diabetes?
Yes, for most people without heart or kidney disease, metformin remains the first-line choice because it’s effective, safe, and affordable. It lowers blood sugar without causing weight gain or hypoglycemia. But if you have cardiovascular disease, obesity, or can’t tolerate metformin, GLP-1 agonists are now recommended as an early alternative-even as a first drug in some cases.
Why are sulfonylureas falling out of favor?
Sulfonylureas cause frequent low blood sugar and weight gain, both of which increase long-term health risks. They don’t protect the heart or kidneys like newer drugs do. Studies show patients on sulfonylureas have higher rates of hospitalization for hypoglycemia and worse outcomes over time. While they’re cheaper, the hidden costs-emergency visits, weight-related complications, and reduced quality of life-often outweigh the savings.
Can I switch from metformin to a GLP-1 agonist if I can’t tolerate the side effects?
Absolutely. If metformin causes severe diarrhea or nausea that doesn’t improve with extended-release versions, switching to a GLP-1 agonist is a valid option. Many patients find the nausea from GLP-1 drugs easier to manage over time, especially with slow dose increases. Plus, the added benefits of weight loss and heart protection often make the trade-off worthwhile.
Are GLP-1 agonists safe for people with kidney problems?
Most GLP-1 agonists are safe even with reduced kidney function. Unlike metformin and sulfonylureas, they don’t rely on kidney clearance as heavily. Dulaglutide (Trulicity) may need a dose adjustment if eGFR falls below 30, but others like semaglutide and liraglutide can be used safely down to stage 4 kidney disease. Always check with your doctor, but kidney issues are no longer a hard barrier to GLP-1 therapy.
Why do some people say GLP-1 agonists cause pancreatitis?
Early animal studies raised concerns, but large human trials have not confirmed a real increase in pancreatitis risk. The FDA reviewed over 50,000 patient-years of data and found no significant link. Nausea and vomiting are common side effects, but true pancreatitis is extremely rare. If you have a history of pancreatitis, your doctor may avoid GLP-1 agonists out of caution-but the risk is very low for most people.
Is there a difference between injectable and oral GLP-1 agonists?
Yes. Injectable versions (like Ozempic) are more potent and have more long-term data. Oral semaglutide (Rybelsus) is slightly less effective at lowering HbA1c and must be taken on an empty stomach with plain water-no food, coffee, or other meds for 30 minutes after. Adherence is higher with the pill, though, because people prefer not to inject. The choice often comes down to effectiveness versus convenience.
Can I stop taking my diabetes medication if I lose weight and improve my diet?
Some people can. If you lose significant weight, improve your diet, and increase activity, you may be able to reduce or stop medication-especially if you’re on metformin or a GLP-1 agonist. But this requires close monitoring. Stopping without medical supervision can lead to dangerous blood sugar spikes. Always work with your doctor to safely taper off, and keep checking your HbA1c regularly.