Workplace Depression Symptom Checker
Symptom Assessment
Select symptoms observed over the past 2 weeks (minimum 2 for meaningful assessment)
Assessment Results
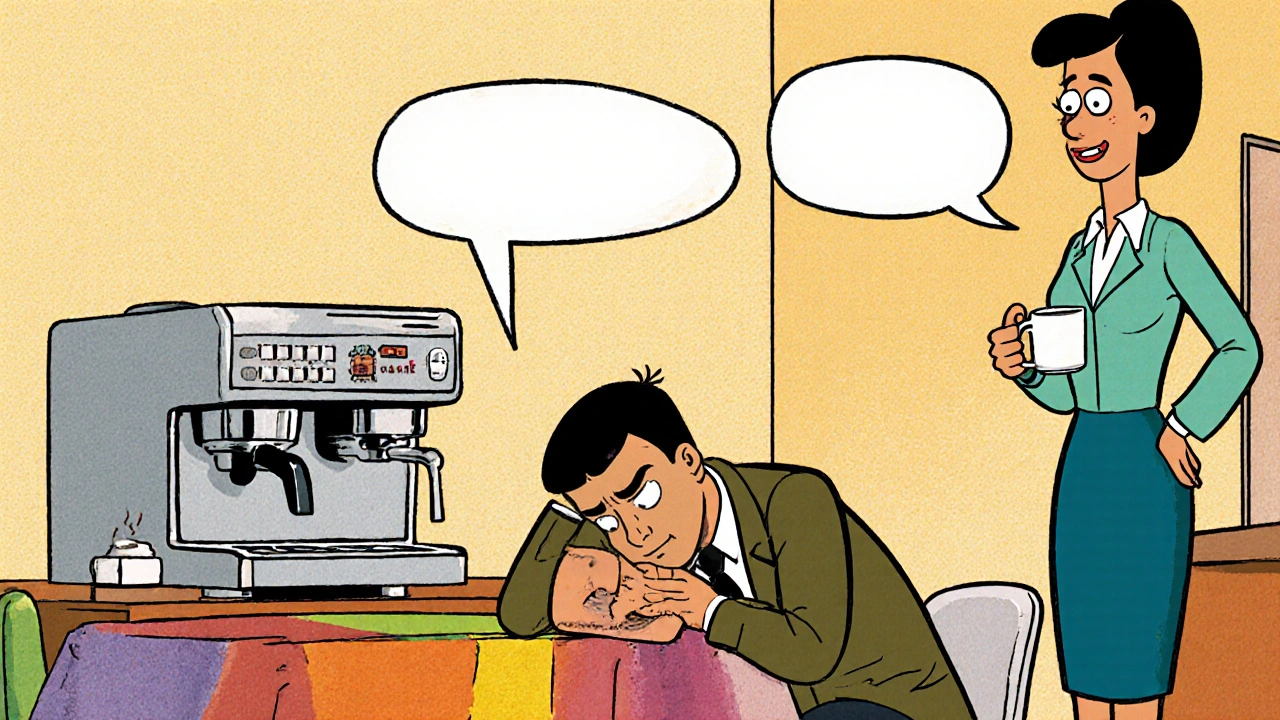
Imagine a colleague who used to share jokes in the break room now barely replies to emails and seems exhausted even after a full night’s sleep. That shift could be more than just a bad day-it might be a sign of depression symptoms workplace. Spotting depression early can save a career, protect team morale, and keep productivity on track.
What is Depression in the Workplace?
Depression is a medical condition characterized by persistent feelings of sadness, loss of interest, and a range of physical and cognitive symptoms that interfere with daily functioning. According to the DSM-5, a formal diagnosis requires at least five symptoms lasting two weeks or more. When these symptoms show up at work, they often blend with normal job stress, making them harder to notice.
Why Does Depression Hide at Work?
Employees may mask depressive feelings for several reasons:
- Stigma: Admitting to mental health struggles can feel risky.
- Job security: Fear of being labeled “unreliable” may keep people silent.
- Professional identity: Many people equate being busy with being competent.
Because of these pressures, depression can masquerade as simple fatigue or lack of motivation, slipping past managers who aren’t trained to look deeper.
Core Symptoms to Watch For
Below are the most common indicators that an employee might be experiencing depression. Not every sign means a diagnosis, but a pattern should raise concern.
- Persistent low mood - a visible “down” attitude that lasts days, not just moments.
- Loss of interest in tasks that once excited them.
- Significant changes in energy levels: chronic fatigue or restless agitation.
- Difficulty concentrating, leading to missed details or errors.
- Changes in appetite or weight, often reflected in erratic lunch habits.
- Increased irritability or frequent conflicts with coworkers.
- Physical complaints without clear medical cause, such as headaches or stomachaches.
- Repeated absences or a trend toward “presenteeism”-showing up but not functioning.
When you see two or more of these symptoms consistently, it’s time to act.
Depression vs. Normal Workplace Stress
| Aspect | Depression | Typical Stress |
|---|---|---|
| Duration | Weeks to months, often unrelenting | Hours to days, tied to specific events |
| Impact on Performance | Consistent decline, errors, missed deadlines | Temporary dips, rebounds after pressure eases |
| Physical Symptoms | Persistent aches, sleep disturbances, appetite changes | Occasional tension, headaches linked to workload |
| Emotional State | Feelings of hopelessness, emptiness, guilt | Frustration, anxiety, occasional irritability |
| Response to Positive Events | Little to no uplift; joy feels muted | Motivation spikes after successes or breaks |
This side‑by‑side view helps managers differentiate a passing stressful period from a deeper mood disorder that needs professional help.

Common Triggers in the Office
While depression can stem from personal life, certain workplace factors amplify risk:
- Long hours and unrealistic deadlines.
- Isolation-especially in remote or hybrid setups.
- Lack of control over tasks or unclear expectations.
- Negative corporate culture or bullying.
- Poor ergonomics leading to chronic pain, which can fuel low mood.
When these stressors pile up, they often intersect with pre‑existing vulnerabilities, creating a perfect storm for depressive episodes.
Business Impact: Absenteeism, Presenteeism, and Productivity
Depression isn’t just a personal health issue; it directly hurts the bottom line. Studies show that employees with untreated depression miss an average of 4.8 workdays per month and experience a 12‑15% drop in overall productivity when they are present but disengaged (presenteeism). This translates into higher Absenteeism costs, increased turnover, and strained team dynamics.
Moreover, when one team member struggles, morale can ripple through peers, leading to a subtle but measurable decline in Workplace Productivity. Early identification and support can therefore save both human and financial resources.
Practical Steps for Managers and Coworkers
Knowing the signs is only half the battle. Here’s a clear roadmap for responding responsibly:
- Observe and Document: Keep a non‑judgmental log of concerning patterns-dates, behaviors, and any impact on work.
- Choose a Private Setting: Approach the employee one‑on‑one, away from distractions.
- Start with Empathy: Use open‑ended questions like, “I’ve noticed you’ve seemed down lately; how are you feeling?”
- Listen Without Offering Immediate Solutions: Validate their feelings before jumping to fixes.
- Share Resources: Mention the company’s Employee Assistance Program (EAP), health‑insurance mental‑health coverage, and the option to speak with an in‑house Psychologist or external therapist.
- Offer Flexible Arrangements: Temporary reduced hours, remote work, or adjusted deadlines can alleviate pressure.
- Involve Occupational Health (if needed): They can conduct a formal assessment and recommend accommodations.
- Follow Up: Schedule regular check‑ins to track progress and adjust support.
Remember, you’re not a therapist. Your role is to connect the employee with professionals who can diagnose and treat depression.

Building a Supportive Workplace Culture
Prevention works best when the environment itself reduces stigma. Consider these long‑term initiatives:
- Offer mental‑health training for all staff, covering basic signs and how to start conversations.
- Normalize “mental health days” as a legitimate part of sick‑leave policies.
- Create peer‑support groups or buddy systems, especially for remote workers.
- Publish clear guidelines on how to access the Employee Assistance Program and insurance benefits.
- Leadership should model openness-share personal experiences if comfortable, showing that it’s okay to seek help.
When employees see that mental health is valued, they’re more likely to come forward before symptoms become severe.
Quick Checklist for Managers
- Monitor for at least two of the core symptoms over a two‑week span.
- Document observations objectively (date, behavior, impact).
- Set up a private, empathetic conversation.
- Provide EAP and mental‑health resource information.
- Offer flexible work options where feasible.
- Schedule a follow‑up within one week.
- Promote a culture that normalizes mental‑health discussions.
Use this list as a living tool-adapt it to your organization’s size and structure.
Frequently Asked Questions
How can I tell the difference between a bad day and depression?
A bad day usually passes within 24‑48 hours and improves with rest or a break. Depression persists for weeks, involves multiple symptoms (low mood, loss of interest, fatigue, etc.), and doesn’t lift after a good night’s sleep.
Should I confront an employee if I suspect depression?
Yes, but do it privately, with empathy, and without diagnosing. Focus on observed work‑related changes and offer resources, letting them decide what steps to take.
What legal obligations do employers have?
In many jurisdictions, depression qualifies as a disability under workplace discrimination laws. Employers must provide reasonable accommodations-like flexible hours-or risk legal action.
Can remote work increase the risk of depression?
Remote work can heighten isolation and blur work‑life boundaries, both of which are known risk factors. Regular virtual check‑ins and clear expectations help mitigate these risks.
What role does the Occupational Health team play?
Occupational Health can conduct formal assessments, recommend workplace adjustments, and coordinate with external mental‑health providers, ensuring compliance with health‑and‑safety regulations.
Addressing depression at work isn’t a one‑off task; it’s an ongoing commitment to people’s well‑being. By recognizing the signs early, responding with empathy, and fostering a supportive culture, you protect both your team members and your organization’s long‑term success.

Kirsten Youtsey
There is a quiet cabal within corporate boards that prefers to label every dip in morale as “just stress,” thereby shielding a systematic neglect of mental health. By relegating depression to a private matter, they maintain an illusion of invulnerability that benefits the elite few at the top. The language in official memos is deliberately vague, masking the true cost of untreated mood disorders on the bottom line. Moreover, the very metrics used to gauge “productivity” are engineered to punish the vulnerable, rewarding only those who can hide suffering behind a veneer of busyness. This strategic obfuscation ensures that the conversation stays confined to HR workshops rather than prompting structural change. In effect, the workplace becomes a laboratory where the symptoms are observed, catalogued, and ultimately dismissed as peripheral concerns.