Why Breast Cancer Screening Starts at 40
Most women don’t think about breast cancer until they’re told they need a mammogram. But the truth is, breast cancer screening isn’t just a checkup-it’s a life-saving step that starts decades before symptoms appear. In 2026, major health organizations like the U.S. Preventive Services Task Force (USPSTF), the American College of Obstetricians and Gynecologists (ACOG), and the American Cancer Society all agree: women at average risk should begin regular mammograms at age 40.
This wasn’t always the case. Ten years ago, many guidelines pushed screening to age 50. But new data changed everything. Invasive breast cancer is rising faster in women under 50 than in any other group. A 2024 ACOG update reviewed over 120 studies and found that starting at 40 saves more lives than waiting. The numbers don’t lie: screening mammography reduces breast cancer deaths by about 12% across all ages. For women in their 40s, that means catching cancer before it spreads-when treatment is simpler and more effective.
How Often Should You Get Screened?
There’s no one-size-fits-all answer, but most women fall into one of two buckets: annual or every two years.
- The USPSTF recommends biennial (every two years) screening for women aged 40 to 74.
- ACOG says you can choose yearly or every two years, based on your risk and preference.
- The American Cancer Society suggests annual screening from 45 to 54, then switching to every two years if you prefer.
- The American Society of Breast Surgeons strongly recommends yearly mammograms starting at 40.
The difference comes down to trade-offs. Annual screening catches more cancers early but increases the chance of false alarms. Every-two-years reduces those false positives but might delay detection by a year. For women with dense breasts or a family history, annual is usually the better choice. For others, biennial is still effective. The key? Talk to your doctor. Don’t just follow a calendar-follow your risk.
2D vs. 3D Mammography: What’s the Difference?
Not all mammograms are the same. Most women still get 2D mammograms-flat X-ray images of the breast. But 3D mammography, also called digital breast tomosynthesis (DBT), is becoming the new standard.
Here’s how it works: instead of one or two pictures, DBT takes dozens of thin slices through the breast, like flipping through a photo album. This helps doctors see through overlapping tissue, which is especially helpful for women with dense breasts. Studies show 3D mammograms find 15% to 40% more invasive cancers than 2D alone. They also reduce the number of women called back for extra tests by up to 30%.
But here’s the catch: DBT isn’t always covered the same way by insurance. Medicare and most private plans cover one screening mammogram per year, whether 2D or 3D. But some insurers still push back on 3D unless you have dense breasts or a high risk. If your doctor recommends it, ask for a pre-authorization. Don’t assume it’s automatic.
Who Needs Extra Screening?
If you have dense breasts, a family history of breast cancer, or a BRCA mutation, your screening plan changes. You’re not just getting a mammogram-you’re getting a layered approach.
For women with a lifetime risk of 20% to 25% or higher (based on tools like Tyrer-Cuzick or Gail model), guidelines now recommend annual mammograms plus annual breast MRI. MRI is far more sensitive than mammography, especially for young women or those with genetic risks. It’s not perfect-it can find things that aren’t cancer-but it’s the best tool we have for catching aggressive tumors early.
What about dense breasts without other risk factors? This is tricky. The USPSTF says there’s not enough proof to recommend extra tests like ultrasound or MRI for these women. But the American Cancer Society and the Society of Breast Imaging say: if your breasts are dense, talk to your doctor about supplemental screening. Many women with dense tissue have cancers missed on mammograms. A 2025 study in JAMA Oncology showed that adding ultrasound to mammography found 3.7 more cancers per 1,000 women with dense breasts.
When Does Screening Stop?
There’s no magic age when you stop. The rule isn’t about your birthday-it’s about your health.
Most guidelines say: keep screening as long as you’re in good health and have a life expectancy of at least 10 years. That means a 78-year-old woman with no chronic illnesses should still get screened. A 75-year-old with advanced heart disease or dementia? Screening may do more harm than good.
Many women stop screening because they’re told, “You’re too old.” But that’s outdated thinking. Breast cancer risk doesn’t drop after 70-it climbs. About 30% of all breast cancer deaths happen in women over 70. If you’re active, independent, and want to stay that way, screening still matters.
What Happens After a Diagnosis?
Screening finds cancer. Treatment makes the difference.
Once a tumor is found, doctors don’t just jump to surgery. They look at four key things:
- Stage-How big is the tumor? Has it spread to lymph nodes?
- Hormone receptors-Is it estrogen- or progesterone-positive? This tells you if hormone therapy will work.
- HER2 status-Is the cancer fueled by the HER2 protein? If yes, targeted drugs like trastuzumab can be life-changing.
- Genomic tests-Tests like Oncotype DX or MammaPrint analyze the tumor’s genes to predict if chemotherapy will help.
Based on this, treatment plans get personalized. A small, hormone-positive tumor in a 65-year-old might only need surgery and hormone pills. A larger, HER2-positive tumor in a 45-year-old might need chemo, targeted therapy, radiation, and surgery. There’s no “standard” path anymore. It’s a puzzle-and every piece matters.

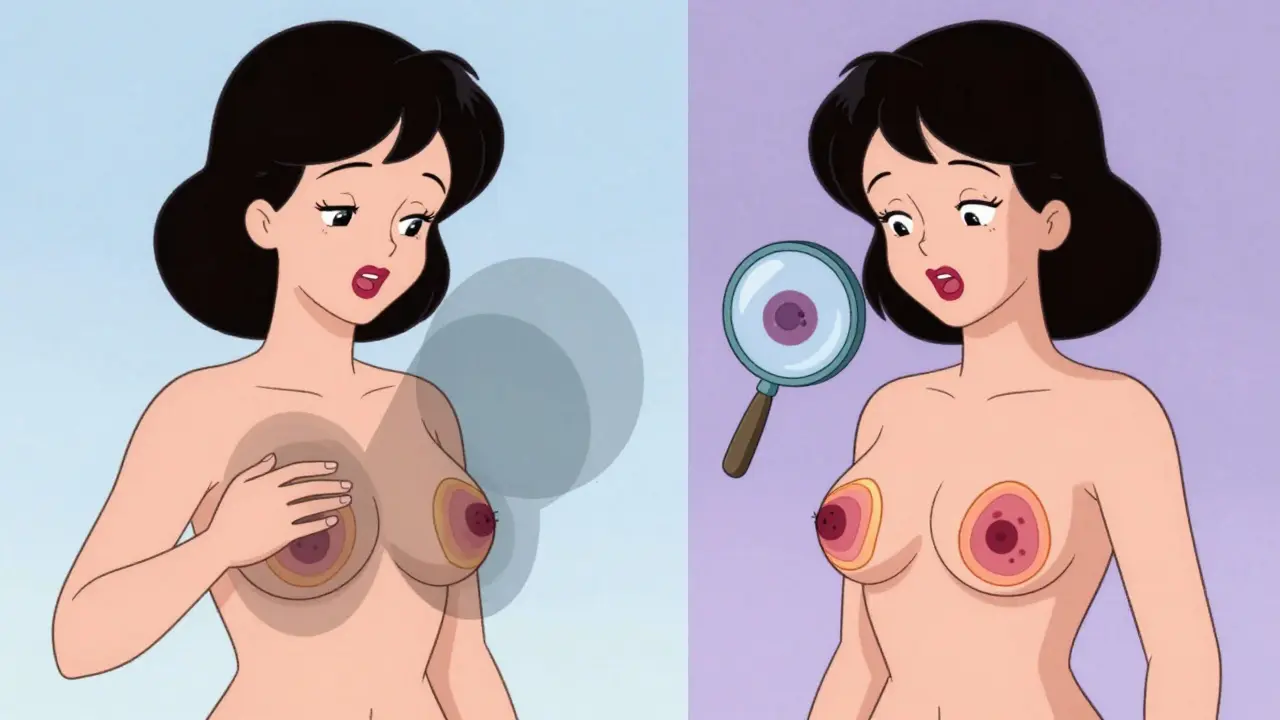
What About Breast Self-Exams?
You’ve probably heard: “Check your breasts every month.” But that advice is fading.
The Canadian Task Force and the USPSTF no longer recommend routine breast self-exams. Why? Multiple studies show they don’t lower death rates-and they lead to more biopsies of harmless lumps. The same goes for clinical breast exams by doctors.
That doesn’t mean ignore your body. If you notice a new lump, nipple discharge, skin dimpling, or pain that doesn’t go away, see your doctor right away. You know your body best. Screening catches what you can’t feel. But your own awareness still matters.
What’s Changing in 2026?
Two big shifts are happening now:
First, AI is helping radiologists. New software can flag suspicious areas on mammograms faster and with fewer errors. Some hospitals are using AI as a second reader-reviewing every scan before the doctor signs off. Early results show a 10% to 15% improvement in cancer detection rates.
Second, screening is becoming more inclusive. More clinics now offer low-cost or free mammograms for uninsured women. Medicaid expansion in 10 states now covers screening starting at 40. And thanks to new federal laws, insurers can no longer charge copays for mammograms-even if they’re 3D.
What Should You Do Next?
If you’re 40 or older: schedule your first mammogram if you haven’t had one. If you’re under 40 and have a family history, ask about risk assessment tools. If you’ve had breast cancer before, talk to your oncologist about ongoing screening.
Don’t wait for symptoms. Don’t assume you’re too young. Don’t skip because you’re nervous. Breast cancer is treatable-especially when caught early. The tools are here. The guidelines are clear. The only thing left is for you to take the step.
Is mammography safe? What about radiation exposure?
Yes, mammography is safe. A standard 2D mammogram uses about 0.4 millisieverts of radiation-less than a chest X-ray and far less than a CT scan. The risk from this tiny amount of radiation is extremely low. The benefit of catching cancer early far outweighs the risk. Modern machines use the lowest possible dose, and technologists are trained to minimize exposure. Women over 40 should not avoid mammograms out of fear of radiation.
What if I have dense breasts?
Dense breasts make mammograms harder to read because both dense tissue and tumors appear white on the image. If you’re told you have dense breasts, ask your doctor about supplemental screening. 3D mammography (DBT) is the best next step. If you’re also at higher risk due to family history or genetics, annual MRI is recommended. Don’t assume a normal 2D mammogram means you’re in the clear-supplemental imaging can find cancers that 2D misses.
Do I need a referral for a mammogram?
No, you don’t need a referral in most cases. Many imaging centers allow women to schedule screening mammograms directly. Check with your insurance first-some plans require prior authorization, especially for 3D mammography. If you’re unsure, call your doctor’s office or your insurer’s customer service line. You have the right to access preventive care without unnecessary barriers.
Can men get breast cancer?
Yes. While rare, about 1 in 833 men will develop breast cancer in their lifetime. Men with BRCA mutations, a strong family history, or conditions like Klinefelter syndrome are at higher risk. Mammograms aren’t routinely recommended for men, but if a man notices a lump, nipple discharge, or skin changes, he should see a doctor immediately. Early detection works for men too.
Are there alternatives to mammography?
For average-risk women, mammography remains the gold standard. Ultrasound and MRI are used as supplements, not replacements. Thermography and breast self-exams alone are not proven to reduce deaths. New technologies like contrast-enhanced mammography and molecular breast imaging are still experimental and not widely recommended. Stick with proven methods: mammography, with MRI added for high-risk cases.

Amy Vickberg
I was diagnosed at 42 and honestly, if I'd waited until 50, I wouldn't be here today. The mammogram that caught it was a 3D scan-my doctor pushed for it even though my insurance initially refused. Got the pre-auth on the second try. Don't let bureaucracy delay your life.
Also, dense breasts? Yes. I had three normal 2D scans before the 3D caught the tumor the others missed. This isn't fear-mongering-it's facts.