Why Your Generic Medicine Might Be Making You Sick
You’ve been taking the same pill for years - brand name, then generic. Same active ingredient, right? So why are you breaking out in hives now? Or feeling dizzy? Or having trouble breathing? If you’ve had a reaction after switching to a generic version of a drug you used to tolerate fine, you’re not alone. And it’s not just in your head.
Generic drugs are required by law to have the same active ingredient as the brand-name version. That’s what makes them cheaper. But here’s what most people don’t know: the rest of the pill - the fillers, dyes, binders, and preservatives - can be completely different. And those differences? They’re what’s triggering allergic reactions in some people.
What’s Really in Your Generic Pill?
Think of a pill like a sandwich. The active ingredient is the meat - the part that treats your condition. But the bread, mustard, pickles, and cheese? Those are the inactive ingredients. They hold the pill together, help it dissolve, make it look nice, or keep it from going bad. In brand-name drugs, these are carefully chosen and consistent. In generics? Not always.
A 2022 study found that 83% of generic drugs contain at least one inactive ingredient that’s different from their brand-name counterpart. Some of these ingredients are common allergens:
- Lactose - found in 28% of oral generics. If you’re lactose intolerant, this can cause bloating, cramps, or worse.
- Gluten - present in 12% of generics. For people with celiac disease, even tiny amounts can trigger serious gut damage.
- Tartrazine (Yellow No. 5) - a bright yellow dye used in 15% of liquid generics. It’s linked to hives, asthma, and swelling in sensitive people.
- Peanut oil - quietly used in some injectable generics. For those with peanut allergies, this can be life-threatening.
One patient in California had a known penicillin allergy and always tolerated brand-name amoxicillin. When switched to the generic, she broke out in hives and swelling. Testing revealed it wasn’t the penicillin - it was a different form of magnesium stearate used in the generic version.
How to Tell If It’s an Allergy - Not Just Side Effects
Not every bad feeling after a pill is an allergy. Nausea from antibiotics? That’s a common side effect. But if your body is having an immune response, that’s an allergy - and it can get worse with every exposure.
Here’s how to spot the difference:
- Mild reactions: Itchy skin, rash, hives, redness. These usually show up within minutes to hours.
- Moderate reactions: Swelling of lips, face, or tongue; wheezing; nausea or vomiting; dizziness. These involve more than one body system.
- Severe reactions (anaphylaxis): Tight throat, trouble breathing, rapid pulse, sudden drop in blood pressure, passing out. This is a medical emergency.
According to data from the American College of Allergy, 43% of severe reactions to generics happen within 15 minutes of taking the pill. Another 38% show up between 15 and 60 minutes. Some, especially with skin rashes, can take hours or even days - but they still count.
When to Call 911 - Not Wait It Out
If you take a generic and feel any of these, don’t wait. Don’t take an antihistamine and hope it goes away. Call emergency services immediately:
- Swelling in your throat or tongue
- Wheezing or gasping for air
- Feeling faint, dizzy, or like you’re going to pass out
- Fast heartbeat or cold, clammy skin
- Two or more symptoms at once - like hives + nausea + swelling
Epinephrine is the only thing that can stop anaphylaxis. If you’ve had a serious reaction before, your doctor should have given you an epinephrine auto-injector. Carry it with you. Know how to use it. And if you use it - even if you feel better - go to the ER. The reaction can come back.

What to Do After a Mild Reaction
If you get a rash or mild itching after switching to a generic, don’t ignore it. It might seem small, but studies show 65% of people who have a mild reaction to a generic will have a worse one next time.
Here’s what to do:
- Stop taking the medication.
- Call your doctor within 24 hours. Don’t wait.
- Write down the exact name of the drug - brand or generic - and the pharmacy you got it from.
- Take a photo of the pill or the prescription label. Generic pills look different depending on the manufacturer.
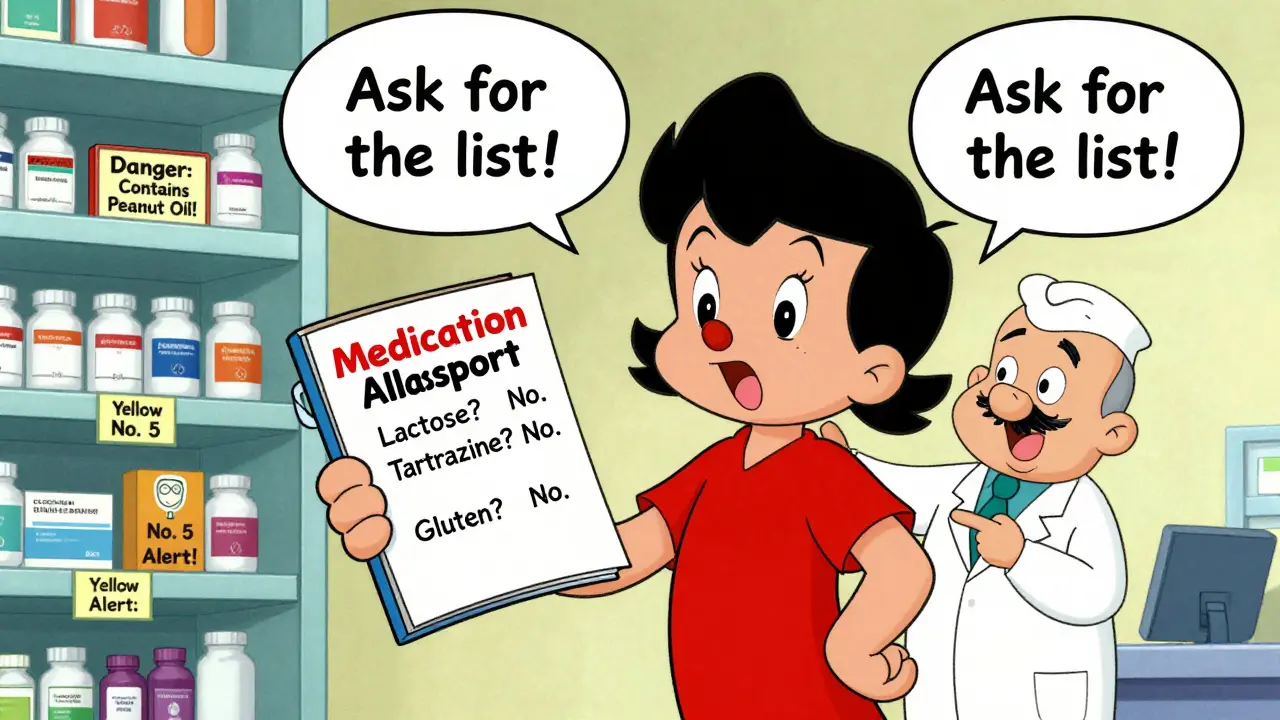
- Ask your pharmacist for the list of inactive ingredients. They’re required to provide it.
Even if you think it was just a coincidence, get it checked. You might be allergic to tartrazine, lactose, or something else that’s hiding in the pill.
How to Avoid Future Reactions
You don’t have to avoid generics forever. But you do need to be smarter about them.
- Ask for dye-free, gluten-free, or lactose-free versions. About 38% of major generic makers now offer these. They’re not always advertised, so you have to ask.
- Keep a ‘medication allergy passport.’ Write down every ingredient you’re allergic to - not just the drug name. Example: ‘Allergic to tartrazine (Yellow No. 5) and lactose.’ Show this to every pharmacist and doctor.
- Stick with the same generic manufacturer. If you’ve had a reaction to one brand of generic, don’t assume another will be safe. Different companies use different fillers.
- Request the brand-name version if you’re at risk. If you have a known allergy to common fillers, your doctor can write ‘Dispense as Written’ or ‘Do Not Substitute’ on your prescription.
- Get tested. An allergist can do skin or blood tests to confirm whether your reaction was truly allergic - and to what ingredient. Many people are mislabeled as allergic to penicillin when they’re really reacting to a dye or binder.
Why Doctors and Pharmacists Don’t Always Know
Here’s the frustrating part: many doctors and even pharmacists don’t check inactive ingredients. They assume if the active drug is the same, the pill is the same.
A 2023 survey found that 41% of pharmacists have had at least one patient each month react to a generic because of an unknown filler. And 15-20% of these reactions go unreported because no one connects the dots.
The FDA requires manufacturers to list inactive ingredients on the package insert - but that’s not always easy to find. Most patients never read it. And if they do, they don’t know what tartrazine or magnesium stearate means.
That’s why your job matters. You’re the one taking the pill. You’re the one who knows your body best. If something feels off after a switch, speak up.
What’s Changing - And What’s Not
The FDA is pushing for better labeling of problematic ingredients in generics by 2025. But until then, you can’t wait for the system to fix itself.
Some hospitals and clinics now use electronic alerts to flag known allergens in prescriptions. But most community pharmacies don’t have that tech yet. And insurance companies often push for the cheapest generic - even if it contains your allergen.
The good news? More allergists are asking patients: ‘Have you had any reactions when switching to generics?’ That question was rare in 2019. Now it’s standard.
Real Stories, Real Risks
A woman in Texas switched from brand-name sertraline to a generic and broke out in hives within 30 minutes. She thought it was stress - until she checked the label. The generic had tartrazine. The brand didn’t. She’s now allergic to every generic SSRI with that dye.
A man with a peanut allergy received a generic version of propofol - an anesthetic - during surgery. It contained peanut oil. He went into anaphylaxis on the operating table. He survived, but only because the team recognized it fast.
These aren’t rare. They’re preventable.
Final Advice: Know Your Pills
Generics save money. That’s great. But they’re not all the same. And for some people, the difference in fillers can be dangerous.
Don’t assume safety just because it’s cheaper. Don’t assume your doctor knows what’s in it. And don’t brush off a rash or itch as ‘just a side effect.’
Here’s your action plan:
- If you’ve had any reaction after switching to a generic - even mild - talk to your doctor.
- Get the list of inactive ingredients from your pharmacist.
- Keep a written record of what you’re allergic to - not just the drug, but the filler.
- Ask for dye-free, gluten-free, or lactose-free versions when possible.
- Carry your epinephrine if you’ve had a serious reaction.
- Don’t take the next generic unless you know what’s in it.
Your health isn’t a cost-saving experiment. It’s your life. And you have the right to know what’s inside every pill you swallow.
Can generic medications cause allergic reactions even if the brand-name version didn’t?
Yes. While the active ingredient is the same, generics often use different inactive ingredients like dyes, lactose, gluten, or peanut oil. These can trigger allergies in people who tolerated the brand-name version just fine. Studies show over 7% of drug allergy reactions are tied to these differences.
What are the most common allergens in generic medications?
The top culprits are lactose (in 28% of oral generics), gluten (12%), tartrazine (Yellow No. 5 dye, in 15% of liquid forms), and peanut oil (in some injectables). These are not always listed clearly on packaging, so patients need to ask pharmacists for the full ingredient list.
When should I go to the emergency room for a reaction to a generic drug?
Go to the ER or call 911 immediately if you experience throat tightness, trouble breathing, swelling of the face or tongue, dizziness, fainting, or a sudden drop in blood pressure. If two or more body systems are affected - like hives plus nausea or wheezing - that’s a sign of anaphylaxis and requires emergency epinephrine.
Can I just take an antihistamine like Benadryl instead of going to the hospital?
Only for mild symptoms like a rash or itching that doesn’t spread or worsen. If there’s any breathing difficulty, swelling, or dizziness, antihistamines won’t stop a severe reaction. Epinephrine is the only treatment for anaphylaxis. Delaying it can be deadly.
How can I find out what’s in my generic medication?
Ask your pharmacist for the full list of inactive ingredients. They can look it up in the FDA’s Inactive Ingredient Database or provide the package insert. You can also search the drug name plus ‘inactive ingredients’ online, but always confirm with your pharmacist - online sources aren’t always accurate.
Should I avoid all generic medications if I have allergies?
No. Many people safely use generics. But if you have known allergies to common fillers like lactose, gluten, or dyes, you need to be proactive. Ask for formulations without those ingredients. Some manufacturers offer ‘free-from’ versions. You can also ask your doctor to write ‘Dispense as Written’ on your prescription to prevent substitution.
Is it safe to switch back to the brand-name version?
Yes, if you’ve had a reaction to a generic and the brand-name version worked fine for you before. Insurance may require prior authorization, but your doctor can explain the medical necessity. Many patients with severe allergies rely on brand-name drugs for safety - and that’s a valid, medically supported choice.
Can I get tested to find out what I’m allergic to in medications?
Yes. Allergists can perform skin tests or blood tests to identify reactions to specific inactive ingredients. This is especially important if you’ve had multiple reactions or are unsure what triggered them. Testing can prevent unnecessary avoidance of safe medications and help you choose safer generics in the future.

Rob Webber
This is pure bullshit. The FDA regulates generics to be bioequivalent. If you're having reactions, it's either psychosomatic or you're just allergic to saving money. Stop blaming the system and start taking responsibility for your own body.