When you’re told your child is allergic to peanuts, or you’ve avoided eggs for years because a skin test said so, how do you know it’s really true? Many people live with food restrictions based on tests that aren’t reliable. That’s where an oral food challenge comes in - the only test that can give you a definite answer.
Why Oral Food Challenges Are the Gold Standard
Skin prick tests and blood tests for IgE antibodies are common, but they’re not perfect. They often say ‘yes’ when the answer is ‘no.’ Studies show these tests have a positive predictive value of just 50-60% for common allergens like peanut or egg. That means half the time, someone is told they’re allergic when they’re not. The result? Unnecessary diets, anxiety, and missed nutrition. An oral food challenge (OFC) cuts through the noise. It’s not a guess. It’s a real test: you eat the food, slowly, under medical supervision, and your body shows you the truth. If you react, you’re allergic. If you don’t, you’re not. The American Academy of Allergy, Asthma & Immunology (AAAAI) and the European Academy of Allergy and Clinical Immunology (EAACI) both call it the gold standard. Why? Because nothing else gives you this level of certainty. It’s not just about confirming allergies - it’s also about ruling them out. About 65% of children outgrow milk or egg allergies by age five. Without an OFC, families might avoid those foods for years, even decades, thinking the allergy still exists. One parent on a food allergy forum said, “My son cried through the whole peanut challenge. But when he ate the full serving without a reaction? We cried too. We got our lives back.”How an Oral Food Challenge Works
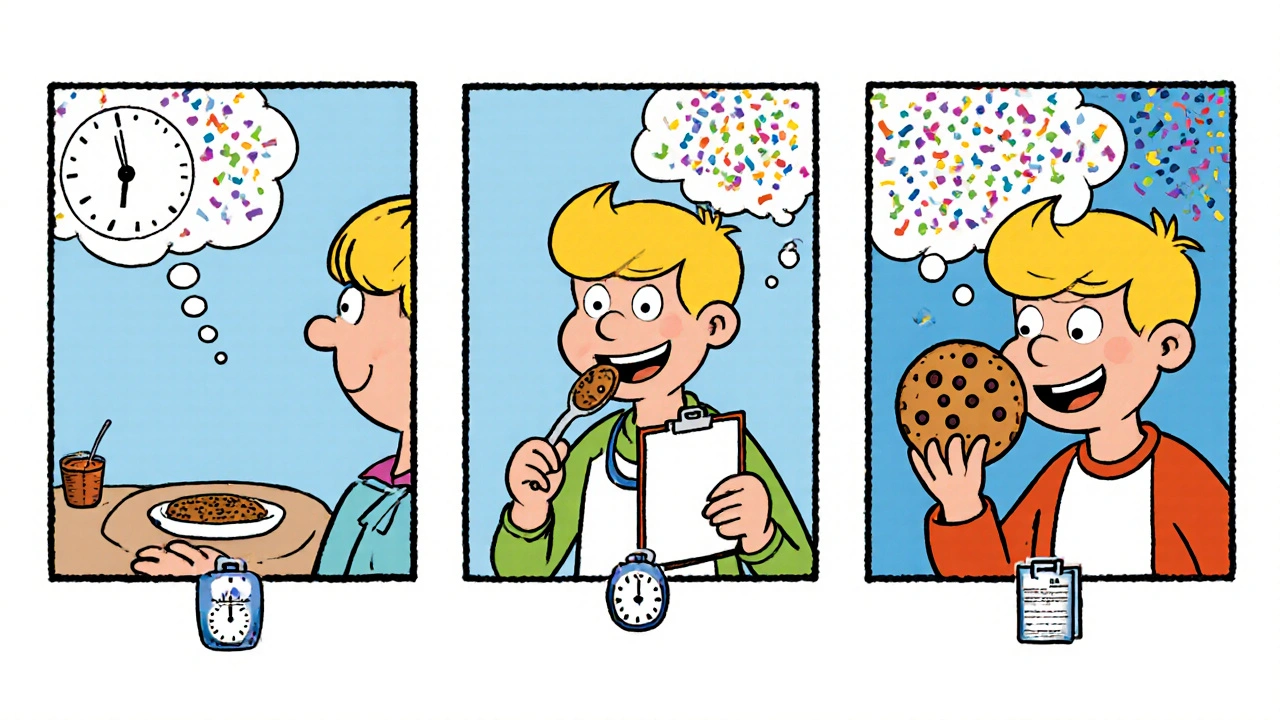
An OFC isn’t a quick snack test. It’s a carefully controlled medical procedure that takes 3 to 6 hours. You start with a tiny amount - often just 1-2 milligrams of the allergen. That’s less than a grain of rice for peanut butter. Each dose increases gradually, usually every 15 to 30 minutes. The goal? To reach a full serving size or until a reaction occurs. The food can be given in different ways. Sometimes it’s pure - like a spoonful of peanut butter. Other times, it’s hidden in a cookie or muffin to reduce anxiety, especially in kids. In rare cases, it’s encapsulated so you can’t taste or smell it. Most challenges (about 90%) are open, meaning both you and the doctor know what’s being given. Blinded tests - where no one knows if it’s the real food or a placebo - are mostly used in research. You’re watched the whole time. Vital signs are checked. Skin is looked at for hives. Breathing is monitored. Nurses and doctors are trained to spot even subtle signs of a reaction - not just full-blown anaphylaxis, but the early warnings like a flushed face, itchy mouth, or mild stomach upset.Who Should Have an Oral Food Challenge?
Not everyone needs one. But if your history is unclear, or test results are mixed, it’s the next step. Common reasons include:- Confirming a suspected food allergy after a mild or unclear reaction
- Testing if a child has outgrown a known allergy (like milk, egg, or soy)
- Clarifying a false positive from a skin or blood test
- Identifying the smallest amount of food that triggers a reaction (the threshold)
Safety: What Are the Real Risks?
Fear keeps people from getting tested. But the data shows OFCs are safer than most assume. About 40-60% of challenges result in mild reactions - usually hives, itching, or a runny nose. These are treated quickly with antihistamines and resolved within minutes. Severe reactions requiring epinephrine happen in only 1-2% of cases, and only when protocols are followed. A 2020 study in the Journal of Allergy and Clinical Immunology found just 0.9% of challenges led to treatment-requiring reactions. That’s lower than the risk of a car ride to the clinic. Clinics must be ready. Epinephrine, oxygen, IV fluids, and steroids must be on hand. At least two trained staff - one doctor, one nurse - must be present. The AAAAI requires this. If a clinic doesn’t meet these standards, they shouldn’t be doing OFCs.What Happens Before and After
Preparation matters. You must stop antihistamines 5-7 days before the challenge. They can hide symptoms and make the test useless. If you’re sick with a cold or asthma flare-up, the challenge gets postponed. Illness can make reactions worse. On the day, wear loose clothes. Bring distractions - tablets, books, favorite toys. Kids (and adults) do better when they’re calm and distracted. Parents are often more anxious than the child. That’s normal. One survey found 78% of caregivers felt moderate to high stress before the test. Afterward, if the challenge is negative - meaning no reaction - you can start including the food in your diet. No more fear. No more hidden ingredients. If it’s positive, you get a clear plan: avoid it, carry epinephrine, and know how to respond.Why Other Tests Can’t Replace It
Newer blood tests like component-resolved diagnostics (CRD) look at specific proteins in food, like Ara h 2 in peanuts. They’re more precise than traditional IgE tests and can predict severity. But even the best CRD tests are only about 85% accurate. That’s good - but not perfect. Only an OFC can tell you if your body will actually react when you eat the food. Allergies aren’t just about antibodies. They’re about how your immune system behaves in real life. A blood test can’t replicate that. That’s why the EAACI says, “No in vitro test can replace the oral food challenge for definitive diagnosis.”
Who Performs Oral Food Challenges?
This isn’t something a general practitioner does. It requires specialized training. The AAAAI recommends doctors complete at least 10 supervised challenges before doing them alone. Most are done in allergy clinics at major hospitals - Cleveland Clinic, Mayo Clinic, Children’s Hospital of Philadelphia - or by board-certified allergists in private practice. In the U.S., about 1.6 to 3.2 million OFCs are performed each year, out of 32 million people with food allergies. That’s still only 5-10% of those who could benefit. Many people never get tested because they don’t know it’s an option - or they’re afraid of the risk.What’s Changing in 2025
New guidelines from the AAAAI in early 2023 now allow home-based OFCs for low-risk cases, under strict conditions. For example, if a child has a history of mild reactions to baked milk and is now being tested to see if they’ve outgrown it, a doctor might approve a supervised home challenge with clear instructions and emergency contact protocols. The NIH is funding research to standardize dosing for high-risk foods like tree nuts. The goal? Reduce reaction rates even further. Meanwhile, experts agree: OFCs will remain the gold standard for years to come. No blood test, no algorithm, no AI model can match the real-time, physiological data you get from someone eating a food and reacting - or not.Real Impact: Life After the Challenge
The real value isn’t just medical. It’s emotional. It’s freedom. One mother in Perth told me her daughter avoided dairy for six years because of a positive blood test. She was malnourished, anxious, and couldn’t eat birthday cake. After an OFC confirmed she was no longer allergic, she gained weight, joined soccer, and ate ice cream for the first time since she was two. Another father said, “We thought we were being careful by avoiding peanuts. Turns out, we were just limiting our lives. The challenge didn’t just test my son’s allergy - it tested our fear.” OFCs don’t just diagnose allergies. They end unnecessary restrictions. They restore confidence. They give families back their meals, their holidays, their peace of mind.If you or your child have a suspected food allergy and the diagnosis is uncertain - talk to an allergist. Ask about an oral food challenge. It’s not a last resort. It’s the best first step to knowing the truth.
Are oral food challenges safe for children?
Yes, oral food challenges are safe for children when done in a properly equipped clinic with trained staff. Mild reactions like hives or stomach upset are common, but severe reactions requiring epinephrine occur in only 1-2% of cases. Most children tolerate the process well, especially when parents use distractions and prepare them emotionally. Clinics that specialize in pediatric allergies have protocols designed to reduce anxiety and ensure safety.
How long does an oral food challenge take?
An oral food challenge typically takes 3 to 6 hours. The first 1-2 hours involve gradually increasing the amount of food given, with doses spaced 15-30 minutes apart. After the final dose, the patient is monitored for another 2-3 hours to watch for delayed reactions. Even if no reaction occurs, the full time is needed to ensure safety.
Can I eat normally before the challenge?
No. You must avoid antihistamines for 5-7 days before the challenge, as they can mask allergic reactions. You should also avoid the suspected food for at least 2 weeks unless otherwise directed. On the day of the test, eat a light meal, stay hydrated, and avoid being sick or having an asthma flare-up - these can increase the risk of a reaction.
What if I react during the challenge?
If you react, the challenge stops immediately. Medical staff will treat the reaction on the spot with medications like antihistamines, steroids, or epinephrine if needed. Most reactions are mild and resolve quickly. Even if you react, the test still gives you valuable information: you’re allergic, and now you know how much triggers your response. This helps tailor your long-term management plan.
Do I need to bring anything to the challenge?
Yes. Bring distractions for children - tablets, books, toys, or favorite snacks (that aren’t the challenge food). Wear loose, comfortable clothing. If you’re a parent, bring a change of clothes in case of a reaction. Also bring your epinephrine auto-injector, even if you’re being tested to see if you still need it - it’s a safety backup.
Will my insurance cover an oral food challenge?
Most insurance plans in the U.S. and Australia cover oral food challenges when ordered by a board-certified allergist and performed in a clinical setting. Coverage varies by provider, but since OFC is the recognized gold standard for diagnosis, it’s typically considered medically necessary. Always check with your insurer and the clinic beforehand to confirm.


Conor McNamara
i heard the fda lets pharma companies pick the 'safe' doses for these challenges... like they pick the amount so no one reacts. then they say 'see? safe!' but if you gave real life amounts, half the kids would drop. they dont want you to know the truth. #conspiracy