Bleeding Risk Calculator
This tool calculates your bleeding risk score based on clinical factors. A score of 3 or higher indicates elevated risk when combining SSRIs with anticoagulants.
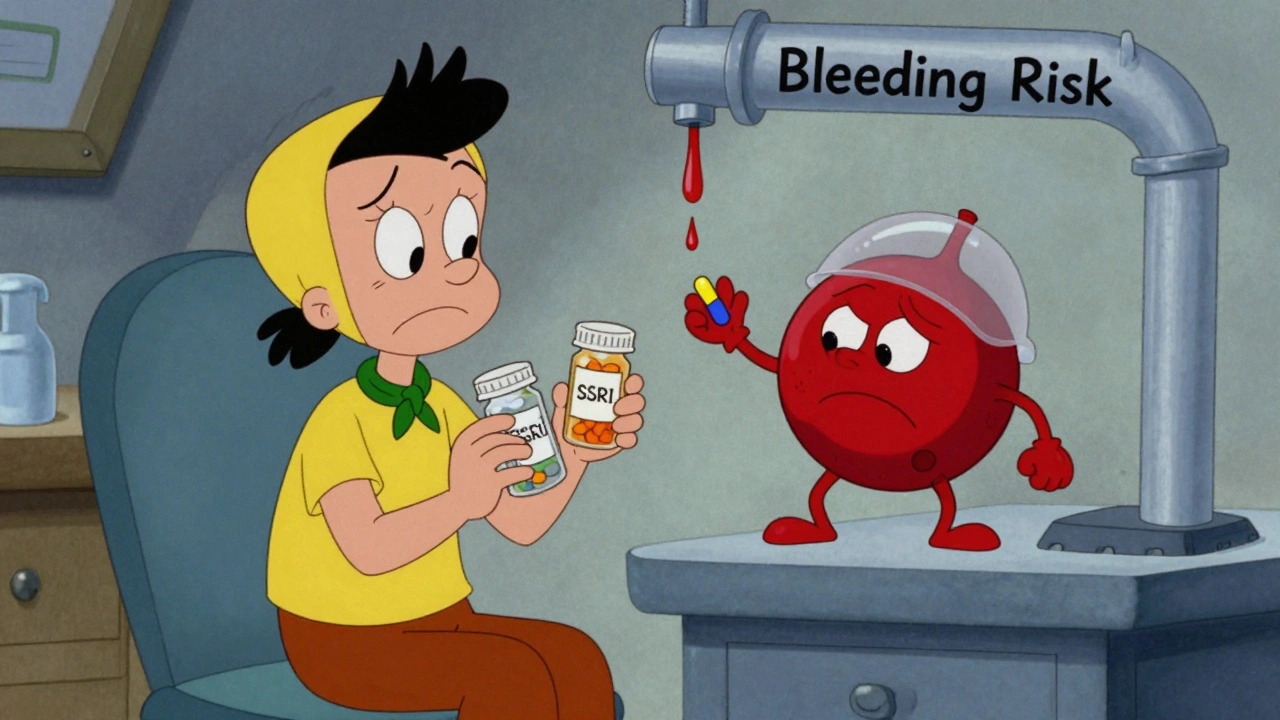
Combining SSRIs with anticoagulants isn’t rare-it’s common. Around 38% of people on blood thinners like warfarin or rivaroxaban also take an SSRI for depression or anxiety. But here’s the thing most patients don’t know: this combo increases your chance of serious bleeding by 33%. That’s not a small risk. It’s enough to change how you and your doctor think about treatment.
Why Does This Happen?
SSRIs don’t thin your blood like aspirin or warfarin. Instead, they mess with your platelets. Platelets are the tiny cells in your blood that clump together to stop bleeding. They need serotonin to work properly. SSRIs block serotonin from re-entering platelets, so those cells end up empty. No serotonin means weaker clots. Studies show this cuts platelet aggregation by 30-40%. It’s like having a team of firefighters who show up but don’t have water. This effect starts the moment you begin taking the SSRI. The biggest spike in bleeding risk happens in the first 30 days. After six months, the risk drops-but it doesn’t disappear. That’s why the FDA added a warning to SSRI labels in 2019 after reviewing 27 serious bleeding cases between 2010 and 2018.Where Does the Bleeding Happen?
It’s not random. Most bleeding events show up in the same places:- Gastrointestinal bleeding (58% of cases): Black stools, vomiting blood, unexplained fatigue
- Intracranial hemorrhage (17%): Sudden headache, confusion, weakness on one side
- Other major bleeding (25%): Nosebleeds that won’t stop, bruising without injury, blood in urine
Not All Blood Thinners Are the Same
The type of anticoagulant matters. Warfarin (a vitamin K antagonist) carries a higher risk when mixed with SSRIs than newer drugs like apixaban or rivaroxaban (DOACs). One 2024 study found:- Warfarin + SSRI: 28% higher bleeding risk
- DOAC + SSRI: 22% higher bleeding risk

Are Some SSRIs Riskier Than Others?
You might think stronger SSRIs like paroxetine are more dangerous. But data says no. The same 2024 study found paroxetine, sertraline, and escitalopram all carried nearly identical bleeding risks. Even though paroxetine blocks serotonin reuptake more powerfully, the real-world outcome was the same. That kills the old myth that “low-potency SSRIs are safer.” Sertraline is still the most prescribed SSRI in this group-not because it’s safer, but because it has fewer drug interactions with other meds. It doesn’t strongly block liver enzymes like CYP2D6 or CYP3A4, which means it’s less likely to interfere with your blood thinner’s metabolism. But again: it still increases bleeding risk.What About Other Antidepressants?
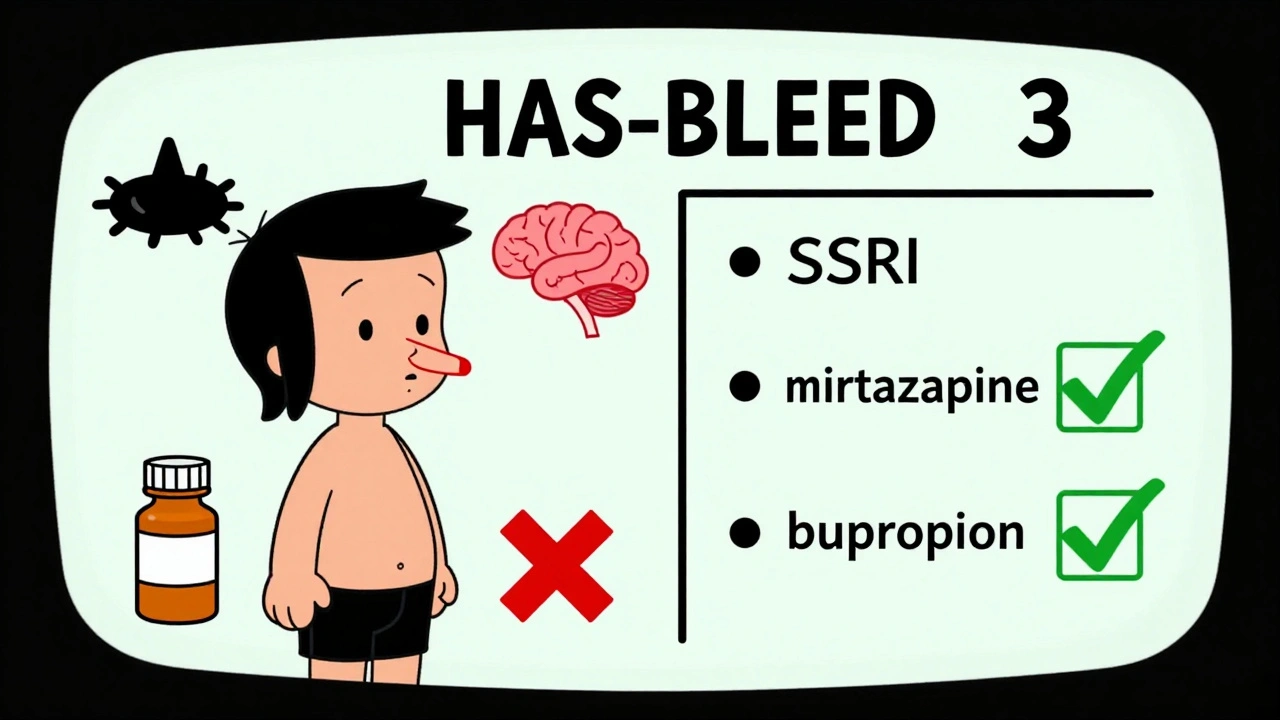
Not all antidepressants carry this risk. Mirtazapine and bupropion don’t affect platelets the same way. They’re often recommended for patients with high bleeding risk-especially those with a HAS-BLED score of 3 or higher (which means they’re already at elevated risk for bleeding due to age, high blood pressure, kidney issues, or past bleeds). The European Heart Rhythm Association says: if you’re on a blood thinner and have a high bleeding risk, consider switching to one of these alternatives. But here’s the catch: SSRIs are still first-line for moderate-to-severe depression in 87% of cases. Why? Because they work. And stopping an SSRI suddenly can trigger withdrawal or worsen depression, which itself increases heart attack and stroke risk.How Do Doctors Monitor This?
If you’re on both, your doctor should be checking for signs of bleeding. That means:- Baseline CBC (complete blood count)
- Fecal occult blood test (to catch hidden GI bleeding)
- Monthly checks for the first three months
- For warfarin users: INR checked twice weekly for the first month
What Should You Do?
If you’re on an anticoagulant and your doctor wants to start an SSRI:- Ask: “What’s my bleeding risk? Is my HAS-BLED score 3 or higher?”
- Ask: “Are there alternatives like mirtazapine or bupropion that won’t increase bleeding?”
- Ask: “Will you check my INR more often if I’m on warfarin?”
- Know the warning signs: unusual bruising, black stools, dizziness, severe headaches
- Don’t stop your SSRI suddenly. Talk to your doctor first.

Carolyn Ford
So let me get this straight: you're telling me my doctor just handed me a time bomb because he thought 'anxiety pill' meant 'harmless'? I've been on sertraline and apixaban for 14 months. No nosebleeds, no black stools... but now I'm Googling every bruise like it's a death sentence. Thanks for the reassurance, doc.