When you’re older, your body doesn’t process medicine the same way it did when you were 30. A pill that once worked perfectly might now make you dizzy, confused, or even sick. That’s not because the drug is broken-it’s because your body has changed. As we age, our organs don’t work the same. Your liver slows down. Your kidneys filter less. Your body holds onto more fat and loses muscle. These changes mean the same dose that was safe at 50 can be dangerous at 75. That’s why medication dosage adjustments for aging bodies and organs aren’t optional-they’re essential.
Why Older Bodies Need Different Doses
Your body’s ability to absorb, distribute, metabolize, and get rid of drugs changes with age. These four steps are called pharmacokinetics. Each one gets slower or less efficient as you get older.First, absorption. Stomach acid drops by 20-30% after age 60. That means some pills don’t break down the same way. Blood flow to your intestines also slows. So even if the drug dissolves, your body takes longer to pull it in.
Then comes distribution. Older adults tend to have more body fat and less muscle. Fat holds onto certain drugs, like benzodiazepines, longer. That means the drug sticks around, building up over time. At the same time, less muscle means less water in your body-so water-soluble drugs like digoxin or lithium become more concentrated. A normal dose can become a toxic one.
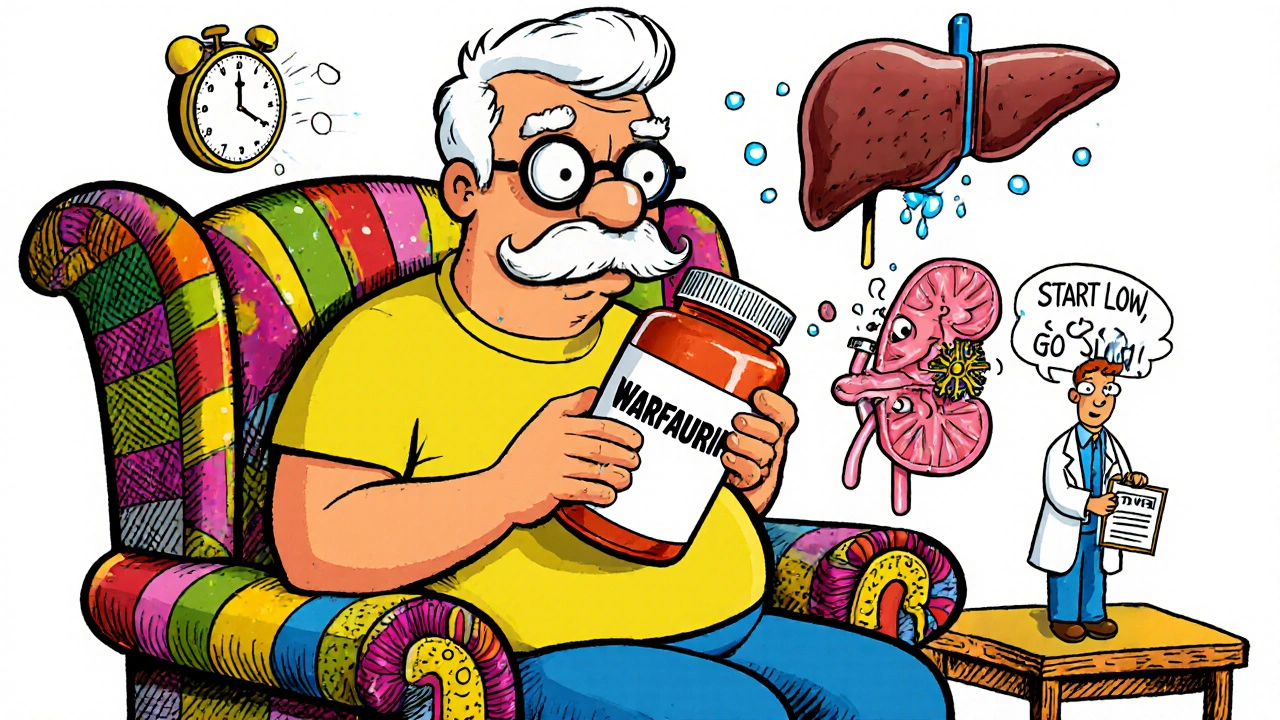
Metabolism is where things get really tricky. Your liver shrinks. Blood flow to it drops. Enzymes that break down drugs slow down. For many medications, liver clearance falls by 30-50%. That’s why drugs like warfarin, statins, or antidepressants need lower doses. Even if your liver looks fine on a scan, its function has declined.
Finally, excretion. Your kidneys do most of the work clearing drugs from your blood. But after age 30, your kidney filter rate (called creatinine clearance) drops about 8 mL per minute every decade. By 70, it’s often half of what it was at 30. Nearly 40% of adults over 65 have kidney function below the level considered normal for adults. That’s why drugs like gabapentin, metformin, or certain antibiotics can build up to dangerous levels if doses aren’t lowered.
The Start Low, Go Slow Rule
Doctors don’t guess at these changes. They follow a clear rule: start low, go slow. It’s been the standard since the 1980s, backed by decades of research from the American Geriatrics Society and the FDA.For example, gabapentin-a common nerve pain drug-is usually started at 300 mg daily for younger adults. For someone over 70, it’s often started at 100 mg. After a week, if there’s no side effects, it might go up to 150 mg. That’s a 50% reduction right off the bat.
Metformin, used for diabetes, is another example. In younger patients, it’s often prescribed at 1,000-2,000 mg daily. But if your kidney function (eGFR) drops below 45, your doctor cuts the dose. Below 30? They stop it. Why? Because metformin builds up in the blood if kidneys can’t clear it, and that can cause a rare but deadly condition called lactic acidosis.
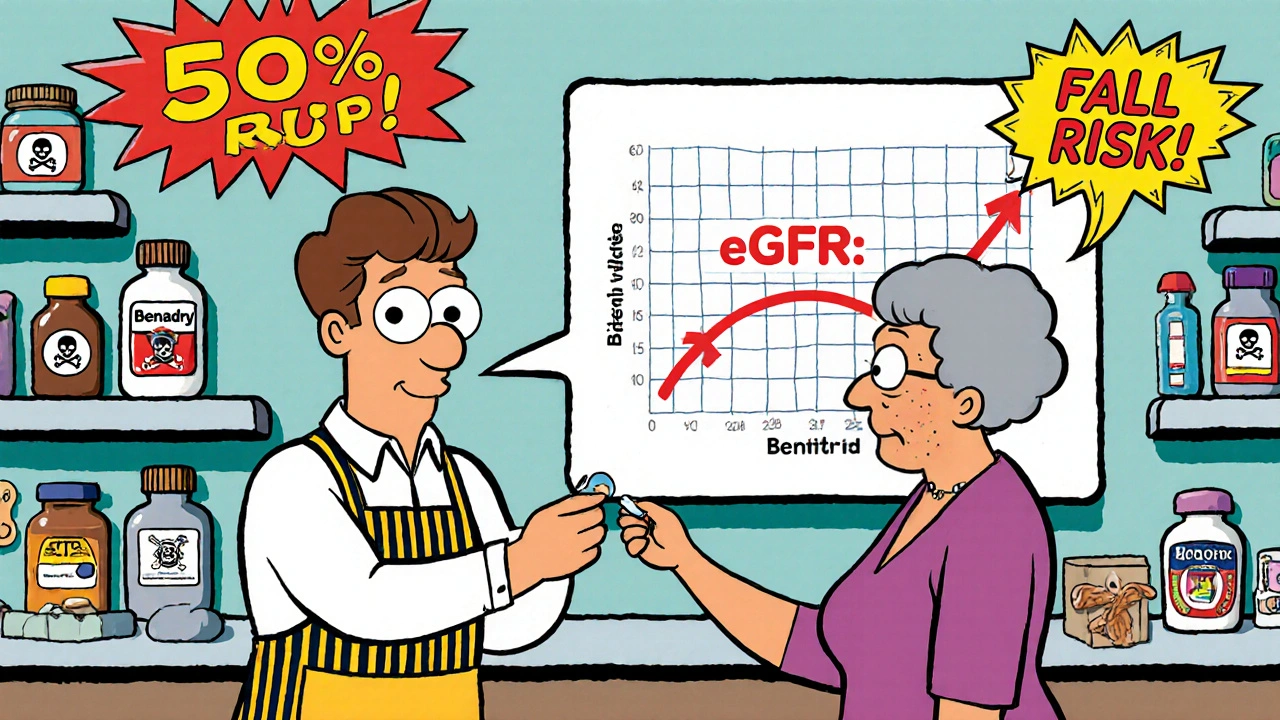
Even something as simple as sleeping pills needs adjustment. Benzodiazepines like lorazepam or alprazolam increase fall risk by 50% in seniors. The standard dose for a 40-year-old might be 1 mg. For someone over 65, 0.5 mg is the max-and even that’s often too much. Many doctors now avoid them entirely.
How Doctors Calculate the Right Dose
There’s no one-size-fits-all formula, but two methods are used most often.The first is the Cockcroft-Gault equation. It estimates how well your kidneys are working based on your age, weight, and blood creatinine level. For men: [(140 - age) × weight in kg] ÷ [72 × serum creatinine]. For women, multiply that result by 0.85. If your result is below 50 mL/min, most kidney-clearing drugs need a 25-50% dose reduction.
The second method is for drugs processed by the liver. The Child-Pugh score looks at things like bilirubin levels, albumin, and fluid buildup. A score of 7-9 (moderate liver trouble) means cut the dose in half. A score of 10-15 (severe) means avoid the drug entirely.
Some drugs, like digoxin, require blood tests to check levels. In younger people, the safe range is 0.8-2.0 ng/mL. In older adults? It’s 0.5-0.9 ng/mL. Too high, and you risk heart rhythm problems. Too low, and it doesn’t work. That’s why doctors don’t just rely on age-they test.
The Biggest Risks in Senior Medications
The 2023 Beers Criteria® from the American Geriatrics Society lists 30 classes of drugs that are risky for older adults. These aren’t just “maybe bad”-they’re proven to cause harm.- Benzodiazepines (like Valium, Xanax): Increase fall risk by 50%. Can cause confusion and memory loss.
- NSAIDs (like ibuprofen, naproxen): Raise risk of stomach bleeding by 300%. Can also wreck kidneys.
- Anticholinergics (like diphenhydramine/Benadryl, oxybutynin): Double the risk of dementia with long-term use.
- Antipsychotics (used off-label for sleep or agitation): Increase stroke risk by 3x in dementia patients.
- Insulin and sulfonylureas (for diabetes): Cause dangerous low blood sugar, which can lead to falls, seizures, or coma.
These aren’t rare side effects. They’re common. In fact, 35% of hospital admissions for people over 65 are due to bad reactions to medications. That’s more than falls, infections, or heart attacks.
What Happens When Dosing Isn’t Adjusted
Take warfarin, a blood thinner. A 75-year-old on the same dose as a 50-year-old might have blood levels twice as high. That’s not a small risk-it’s life-threatening. A single drop in kidney function can turn a safe dose into a bleeding risk.One study found that 27% of adverse drug events in nursing homes came from wrong dosing-not wrong drugs. Anticoagulants, diabetes meds, and blood pressure pills were the top three culprits. Why? Because they have narrow safety margins. A tiny bit too much, and you’re in the ER.
And it’s not just the drugs themselves. Polypharmacy-taking five or more medications-is common in seniors. One study found 55% of adults over 65 take five or more prescriptions. Each one interacts. One drug might slow the liver’s ability to break down another. A blood pressure pill might make a diabetes drug more likely to cause low sugar. It’s a chain reaction.
How to Make Sure Your Dose Is Right
You don’t have to guess. Here’s what works:- Do a brown bag review. Bring every pill, vitamin, and supplement to your doctor. Don’t rely on memory. Many seniors take things they forgot they were on.
- Ask for a kidney test. Get your creatinine and eGFR checked at least once a year. If you’re on any kidney-cleared drug, you need this.
- Ask: Is this still necessary? Many seniors stay on drugs they started years ago. Ask your doctor: “Would you prescribe this today if I were just starting?”
- Use a pharmacist. Pharmacists are trained in geriatric dosing. Many pharmacies now offer free medication reviews. They catch errors doctors miss.
- Track side effects. Write down dizziness, confusion, nausea, or falls. Don’t assume it’s just “getting older.”
Some clinics have success with weekly blister packs and pharmacist-led follow-ups. One program at the University of North Carolina cut hospital visits by 22% just by making sure seniors got the right dose at the right time.
What’s Changing in the Field
The FDA now requires drug trials to include more older adults. In 2010, only 28% of participants in major trials were over 65. By 2022, that jumped to 42%. That’s progress.But there’s still a gap. Most trials still don’t include people over 75-even though they’re the ones most likely to need these drugs. That’s why doctors still have to guess sometimes.
New tools are emerging. AI algorithms can now predict the right dose based on age, weight, kidney function, and other meds. One pilot at Johns Hopkins cut dosing errors by 47%. But these tools aren’t everywhere yet.
Soon, doctors may use more than age to decide doses. Gait speed, grip strength, and memory tests are being studied as better predictors than just a number on a chart. If you can’t walk 12 feet without stopping, your body might need even lower doses-even if your kidneys look fine.
What You Can Do Today
You don’t need to wait for new science. Start now:- Don’t take over-the-counter meds without asking. Benadryl, Pepto-Bismol, and even some cold pills can be dangerous.
- Ask your doctor: “What’s the lowest dose that will work?”
- Don’t stop a drug because you’re afraid. Talk to your doctor first.
- If you’re on more than five meds, ask for a medication review. Many insurance plans cover it.
- Keep a list. Write down every drug, dose, and reason you take it. Bring it to every appointment.
Medication isn’t just about pills. It’s about safety. For older adults, the right dose isn’t just better-it’s life-saving.
Why can’t older adults take the same medication doses as younger people?
Because aging changes how the body handles drugs. Kidneys filter slower, liver breaks down drugs less efficiently, body fat increases, and muscle mass decreases. These changes mean drugs stay in the system longer and at higher concentrations. A dose that’s safe for a 40-year-old can be toxic for a 75-year-old.
What is the Beers Criteria and why does it matter?
The Beers Criteria is a list of medications that are potentially inappropriate for older adults because they carry high risks of side effects like falls, confusion, kidney damage, or dementia. Updated every two years by the American Geriatrics Society, it’s the gold standard for geriatric prescribing. If a drug is on this list, your doctor should avoid it or use extreme caution.
How do I know if my kidney function is low enough to need a dose change?
Your doctor can check your eGFR (estimated glomerular filtration rate) with a simple blood test. If your eGFR is below 60 mL/min/1.73m², your kidneys aren’t working at full strength. If it’s below 45, most kidney-cleared drugs need a reduced dose. Below 30, many should be stopped.
Are over-the-counter drugs safe for seniors?
Not always. Many OTC meds contain anticholinergics (like diphenhydramine in Benadryl or sleep aids) or NSAIDs (like ibuprofen), which are high-risk for seniors. These can cause confusion, urinary retention, falls, or stomach bleeding. Always check with your pharmacist before taking any non-prescription drug.
Can I stop a medication if I think it’s causing side effects?
Never stop a medication without talking to your doctor. Some drugs, like blood pressure or seizure meds, can cause dangerous rebound effects if stopped suddenly. But if you notice dizziness, confusion, nausea, or falls, write it down and bring it to your next appointment. Your doctor may lower the dose or switch you to a safer option.
How often should seniors have their medications reviewed?
At least once a year, or every time you see a new doctor or start a new medication. If you’re on five or more drugs, or have kidney or liver issues, every six months is better. Many pharmacies offer free medication reviews-ask for one.
Next Steps for Safer Medication Use
If you’re caring for an older adult, here’s what to do next:- Get a copy of their full medication list-including vitamins and supplements.
- Call their pharmacy and ask for a medication review. Many offer this for free.
- Ask their doctor for a kidney function test if they’re on any prescription meds.
- Use a pill organizer with alarms if they’re taking multiple daily doses.
- Watch for signs of dizziness, confusion, or unexplained falls. These aren’t normal aging-they’re warning signs.
The goal isn’t to take fewer pills-it’s to take the right ones, at the right dose, for the right reason. In older adults, that’s not just good medicine. It’s the difference between staying independent and ending up in the hospital.

Summer Joy
I swear my grandma took 5 different pills and ended up in the ER because she didn’t tell anyone about the OTC sleep aid she was sneaking. 😤 Now she’s on a blister pack, and her balance is better. Why do we treat seniors like they’re dumb? They just need better systems, not more judgment.