When you’re pregnant and struggling with depression or anxiety, the question isn’t just should I take medication? It’s: What happens if I don’t? For many women, the fear of harming the baby often outweighs the fear of their own mental health crashing. But the truth is, untreated depression during pregnancy carries risks that are just as real - and sometimes more dangerous - than the medications used to treat it.
Why SSRIs Are Even Considered During Pregnancy
Selective Serotonin Reuptake Inhibitors, or SSRIs, are the most commonly prescribed antidepressants for pregnant women. Medications like sertraline (Zoloft), citalopram (Celexa), and escitalopram (Lexapro) have been studied in hundreds of thousands of pregnancies. They’re not perfect, but they’re the best option we have for managing moderate to severe depression when therapy alone isn’t enough. The reason they’re used isn’t because they’re risk-free. It’s because the alternative - leaving depression untreated - is far riskier. Depression during pregnancy isn’t just feeling sad. It can lead to poor nutrition, missed prenatal appointments, substance use, and even suicide. In the U.S., suicide accounts for 20% of all pregnancy-related deaths, according to CDC data from 2022. That’s more than hemorrhage or preeclampsia in some groups.The Real Risks: What the Data Actually Shows
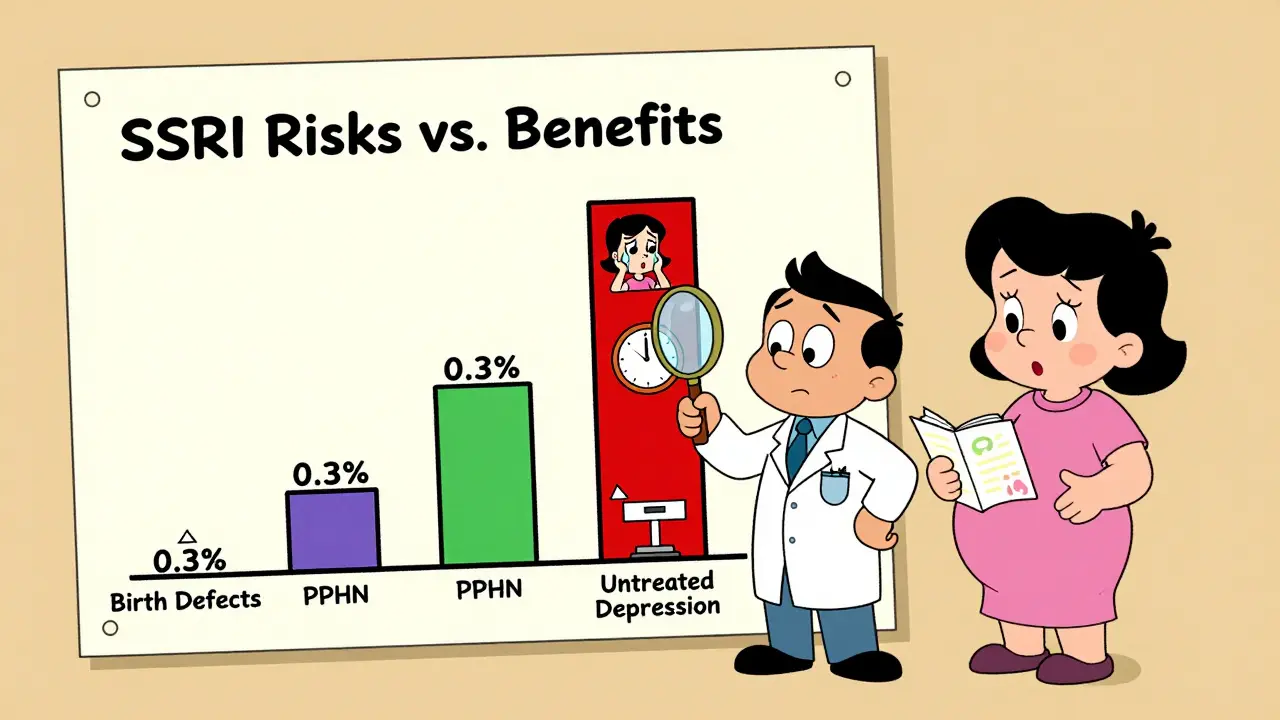
Let’s cut through the noise. There are scary headlines about SSRIs causing birth defects, autism, or lifelong problems. But when you look at the full picture - large, well-designed studies - the risks are smaller than they sound.- Birth defects: The absolute risk of a major congenital malformation in any pregnancy is about 2.5%. With SSRIs, it rises to 2.8%. That’s a 0.3% increase - not a doubling, not a tripling. Paroxetine is the exception: it’s linked to a slightly higher risk of heart defects, which is why it’s avoided in the first trimester.
- PPHN (Persistent Pulmonary Hypertension of the Newborn): This rare but serious lung condition affects 1-2 in 1,000 babies overall. With SSRI use in the third trimester, that number goes up to 3-6 in 1,000. Still, 99.4% of babies exposed to SSRIs in late pregnancy do not develop PPHN.
- Preterm birth and low birth weight: Studies show slightly higher rates among women taking SSRIs. But here’s the catch: women with severe depression who don’t take medication have even higher rates. When researchers adjust for how severe the depression was, the difference almost disappears.
The Bigger Risk: What Happens If You Stop
Many women stop their SSRIs the moment they find out they’re pregnant. It feels safer. But the data says otherwise. A 2022 JAMA Psychiatry study tracked women who stopped SSRIs during pregnancy versus those who kept taking them. The results were stark:- 92% of women who stopped had a relapse of depression.
- Only 21% of those who continued their medication relapsed.
Which SSRI Is Safest?
Not all SSRIs are the same. Sertraline is the go-to choice for most doctors because:- It has the lowest risk of heart defects.
- It crosses the placenta less than fluoxetine or paroxetine.
- It has the lowest reported risk of PPHN.
- It’s been studied more than any other SSRI in pregnancy.
What About Breastfeeding?
Most SSRIs are safe during breastfeeding. Sertraline is the top choice here too - it passes into breast milk in very low amounts. Studies show no significant impact on infant weight gain, sleep, or development. Fluoxetine is less ideal because it builds up in the baby’s system over time. The American Academy of Pediatrics considers sertraline compatible with breastfeeding. The benefits of treating maternal depression usually outweigh any minimal exposure through milk.What If You Want to Stop?
If you’re thinking about stopping, don’t quit cold turkey. Abruptly stopping SSRIs can cause withdrawal symptoms: dizziness (42%), nausea (38%), brain zaps (29%), and severe mood swings. A 2023 study in Obstetrics & Gynecology found that 73% of women who stopped suddenly experienced these symptoms. Instead, work with your doctor. A slow taper over 4-6 weeks, with weekly check-ins using the PHQ-9 depression scale, is the safest approach. If your mood starts to dip during the taper, it’s a sign you still need the medication.Long-Term Effects on the Child
This is where things get complicated. Some studies suggest children exposed to SSRIs in utero may have a slightly higher risk of anxiety or depression by age 15. One 2023 Columbia University study found 28% of exposed children developed depression by adolescence, compared to 12% in children whose mothers had depression but didn’t take medication. But here’s the twist: those same children’s mothers had more severe depression. When researchers adjusted for family history, genetics, and environmental stress, the difference vanished. A 2021 Lancet study found no link between SSRI exposure and autism when they accounted for inherited risk factors. The takeaway? The child’s mental health is shaped more by how well the mother’s depression was managed - and how supported she was - than by the medication itself.
What Doctors Actually Recommend Today
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) both say the same thing in their 2023 guidelines:“For women with moderate to severe depression, the benefits of continuing SSRIs generally outweigh potential risks.”They recommend:
- Start with sertraline at 25-50mg daily, adjust as needed.
- Avoid paroxetine in the first trimester.
- Don’t switch medications unless absolutely necessary.
- Continue treatment through delivery and breastfeeding if it’s working.
Your Next Steps
If you’re pregnant and taking SSRIs:- Don’t stop without talking to your doctor.
- Ask for sertraline if you’re not already on it.
- Get regular mental health check-ins - not just physical ones.
- Know the real numbers: PPHN risk is less than 1% even with SSRIs.
- Remember: treating your depression helps your baby more than you think.
- Therapy helps - but not always enough.
- Medication isn’t a failure. It’s a tool.
- You’re not choosing between your health and your baby’s. You’re choosing the best way to care for both.
Frequently Asked Questions
Are SSRIs safe in the first trimester?
Yes, most SSRIs are considered safe in the first trimester. Sertraline, citalopram, and escitalopram show no significant increase in major birth defects. Paroxetine is the only SSRI linked to a small increase in heart defects, so it’s avoided. The overall risk of any major defect remains under 3%, even with SSRI use.
Can SSRIs cause autism in babies?
Large, well-controlled studies - including one from the Lancet in 2021 that adjusted for genetic and environmental factors - found no meaningful link between SSRI exposure and autism. Some smaller studies suggested a connection, but they didn’t account for the fact that autism risk runs in families. Mothers who take SSRIs often have a history of anxiety or depression, which are linked to autism risk independently of medication.
What if I’m on a different antidepressant?
If you’re doing well on your current medication, don’t switch. The goal is stability. Switching meds during pregnancy can trigger relapse. If you’re on paroxetine, talk to your doctor about switching to sertraline before or early in pregnancy. For other antidepressants like SNRIs or bupropion, safety data is less clear - so stick with SSRIs unless your doctor advises otherwise.
Will my baby have withdrawal symptoms?
About 30% of babies exposed to SSRIs late in pregnancy show mild withdrawal symptoms - fussiness, jitteriness, feeding trouble, or mild breathing issues. These usually last only a few days to two weeks and don’t cause long-term harm. Hospital staff are trained to watch for this and provide supportive care. It’s not the same as addiction.
Is it better to take SSRIs or try natural remedies?
Exercise, sunlight, and therapy help - especially for mild depression. But for moderate to severe depression, they’re not enough on their own. Natural remedies like St. John’s Wort are not recommended during pregnancy - they interact with other medications and lack safety data. SSRIs have been studied in millions of pregnancies. The evidence for their benefit is strong. Don’t trade proven treatment for unproven alternatives when your mental health is at stake.


Rich Robertson
Look, I get the fear. I was pregnant and on sertraline. Everyone kept telling me it was dangerous, but no one told me what happens when you stop. I crashed hard. Didn’t leave the house for three weeks. My husband had to feed me soup with a spoon. The baby was fine. I’m not some medical robot-I’m a mom who needed help, and SSRIs gave it to me.
Stop making this about pills. It’s about survival. If you wouldn’t deny a diabetic insulin, why deny a depressed person an SSRI?