When you’re over 70, taking a pill isn’t just about following the label. It’s about making sure your kidneys can handle it. As we age, our kidneys slowly lose function-not because of disease, but because of time. On average, a 75-year-old has about 40% less kidney filtering power than a 30-year-old. That means drugs that used to be safe at one dose can become dangerous at the same dose today. And it’s not rare. About 30% of medications commonly prescribed to seniors are cleared almost entirely by the kidneys. Miss this, and you risk confusion, falls, kidney damage, or worse.
Why Kidney Function Changes with Age
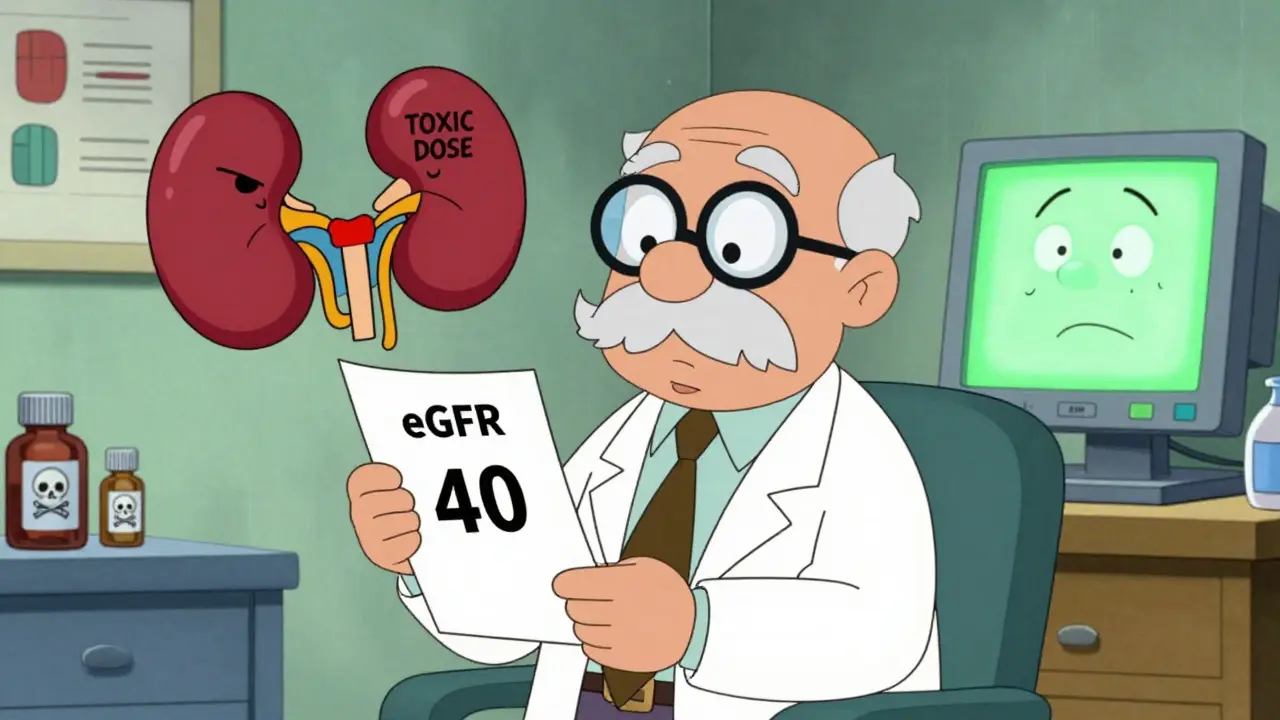
Your kidneys don’t just wear out like old shoes. They lose nephrons-the tiny filters that clean your blood. Blood flow to the kidneys drops. The glomeruli, the filtering units, thicken and scar. By age 70, most people have an estimated glomerular filtration rate (eGFR) of around 75 mL/min/1.73 m². That’s down from 116 in your 20s. It’s normal. But it’s not accounted for in most drug labels.Many prescriptions still assume you’re a healthy 40-year-old. That’s why so many seniors end up with toxic drug levels. Take digoxin for heart rhythm, or gabapentin for nerve pain. Both are cleared by the kidneys. If your eGFR is 40, but you’re still getting the standard dose, you’re basically overdosing. And you might not feel it until you fall, get confused, or end up in the hospital.
The Equations That Matter
Doctors don’t measure kidney function directly. They use equations based on blood tests. The most common one is serum creatinine. But creatinine comes from muscle. And as we age, we lose muscle. So a low creatinine level doesn’t always mean healthy kidneys-it might just mean you’re frail.Here are the three main equations used to estimate kidney function, and why they fall short for seniors:
- Cockcroft-Gault (CG): Uses age, weight, gender, and serum creatinine. It was designed in 1976. It’s old, but it still works well for dosing because it estimates creatinine clearance-the actual amount of drug your kidneys can remove. The trick? Use ideal body weight, not your actual weight. If you’re overweight or underweight, using real weight gives you the wrong dose. Studies show using ideal body weight cuts dosing errors by 15-20%.
- MDRD: Developed in 1999. It’s built for population studies, not individual dosing. It underestimates kidney function in seniors, especially those over 75. It’s often wrong by 10-15 mL/min/1.73 m².
- CKD-EPI: Introduced in 2009. It’s the most widely used today. Most EHR systems default to this. But in very old adults, especially those with low muscle mass, it can overestimate kidney function. That’s dangerous. A patient with an eGFR of 55 on CKD-EPI might actually have a true GFR of 38. That’s a big difference when you’re on blood thinners like rivaroxaban.
There’s a better option for seniors over 75: BIS1 and FAS. These equations were built specifically for older adults. They account for age, sex, and creatinine-but they also adjust for the fact that older people have less muscle. In a 2019 study of 85-year-olds, BIS1 was accurate within 30% of the real GFR in 95% of cases. CKD-EPI? Only 78%. That’s not a small gap. It’s the difference between a safe dose and a toxic one.
When Creatinine Isn’t Enough
If you’re thin, frail, or have had a recent illness, creatinine can lie. That’s where cystatin C comes in. It’s a protein made by all cells, not just muscles. It’s not affected by body weight or diet. A cystatin C-based eGFR is more accurate for frail seniors.Here’s the catch: cystatin C costs $50-$75 more than a standard creatinine test. Most clinics don’t order it routinely. But if your creatinine-based eGFR is 45-59 and you have no signs of kidney disease (no protein in urine, no high blood pressure, no diabetes), then cystatin C is worth asking for. If it’s normal, your kidneys might be fine-and you might not need a dose reduction.
And if you’re on a drug where even a small mistake can kill you-like vancomycin, aminoglycosides, or colistin-doctors should consider a 24-hour urine collection. It’s the gold standard. It’s messy. It takes time. But for high-risk meds, it’s the only way to be sure.

What the Experts Recommend
The American Society of Nephrology says CKD-EPI is fine for most adults. But for seniors over 75? They say: consider BIS1 or FAS. Dr. Sophie Dupont at the University of Michigan Geriatric Kidney Disease Clinic switched her entire team to BIS1 for patients over 80. In their 2023 study, medication-related adverse events dropped by 18%.The American Geriatrics Society doesn’t pick one equation. They say: use clinical judgment. Look at the person-not just the number. Are they eating well? Are they losing weight? Do they walk without a cane? Are they on five or more medications? Those things matter more than any equation.
And here’s the reality: most doctors don’t know which equation to use. A 2022 survey found 65% of primary care physicians are confused. Many just use whatever their electronic health record picks. And if your EHR defaults to CKD-EPI? You’re at risk.
What You Can Do
If you or a loved one is over 70 and on regular medication, here’s what to ask for:- Ask for your eGFR number. Don’t just accept “your kidneys are fine.” Ask: “What’s my number? Which equation was used?”
- Check if it’s CKD-EPI. If you’re over 75, ask: “Could we use BIS1 instead?”
- Ask about ideal body weight. If they’re using Cockcroft-Gault, make sure they’re not using your actual weight. Ideal body weight is calculated as 50 kg for women + 2.3 kg for every inch over 5 feet. For men: 50 kg + 2.3 kg per inch over 5 feet.
- Request cystatin C if your eGFR is borderline (45-59) and you’re frail.
- Review all meds with your pharmacist. Pharmacists in senior care settings are trained to catch these errors. They override EHR defaults weekly. Let them help.
Some hospitals now have smart systems. Epic, for example, automatically switches to BIS1 for patients over 75. But most community clinics don’t. That’s on you to ask.

The Bigger Picture
This isn’t just about one equation. It’s about a system built for young, healthy people. Drug labels, EHR defaults, even medical school training still treat aging as an exception-not the norm. But by 2030, 1 in 5 Americans will be over 65. We can’t keep dosing seniors like they’re 40.That’s why the FDA now requires drug makers to provide dosing guidance using multiple equations. That’s why Medicare is starting to penalize hospitals for medication errors in seniors. And that’s why the National Institute on Aging is funding new research to build better, AI-driven tools that look at muscle mass, nutrition, and comorbidities-not just a single blood number.
For now, the best tool you have is knowledge. Know your numbers. Ask questions. Don’t let a default setting decide your safety.
What to Do If You’re Already on a Problematic Drug
If you’re on a drug with a narrow therapeutic window-like warfarin, digoxin, lithium, or certain antibiotics-and you’ve had side effects like dizziness, confusion, or nausea-you should act.- Get a full medication review with a geriatric pharmacist.
- Ask for a repeat eGFR using BIS1 and cystatin C.
- Check if your dose has been adjusted for kidney function in the last 6 months.
- Don’t assume “it’s been fine for years.” Kidney function changes slowly. What was safe last year might not be today.
One Reddit user shared: “My 88-year-old mom got vancomycin toxicity because her EHR used CKD-EPI. Switching to BIS1 fixed it. She’s back home.” That’s not luck. That’s knowing what to ask for.
How often should seniors get their kidney function checked?
Seniors over 65 with no chronic conditions should have kidney function checked at least once a year. If you have diabetes, high blood pressure, heart failure, or take multiple medications, check every 3-6 months. If you’re hospitalized or start a new kidney-cleared drug, check immediately.
Is CKD-EPI always wrong for seniors?
No. CKD-EPI works well for seniors with normal muscle mass and no frailty. But for those over 75, especially if they’re thin, malnourished, or have multiple illnesses, it often overestimates kidney function. That’s why BIS1 or FAS are better choices in those cases.
Can I use an online calculator to check my eGFR?
Yes, but be careful. The National Kidney Foundation and American Society of Nephrology both offer free online calculators. Make sure the one you use lets you select the equation. If it only shows CKD-EPI, it’s not designed for seniors. Look for options to use Cockcroft-Gault with ideal body weight or BIS1.
What if my doctor says my kidneys are fine but I feel off?
Trust your body. Symptoms like fatigue, confusion, swelling, or nausea can be signs of drug buildup-even if your eGFR looks okay. Ask for a cystatin C test and a full medication review. Your symptoms matter more than a number.
Are there any new tests coming soon?
Yes. The CKD2024 equation, which combines creatinine and cystatin C, is showing 15% better accuracy in people over 80. The National Institute on Aging is also funding point-of-care devices that could measure kidney function in minutes using just a finger-prick blood sample. These tools will soon help doctors make faster, smarter decisions.
Final Thoughts
Safe dosing for seniors isn’t about finding the perfect equation. It’s about asking the right questions. It’s about knowing that your kidneys aren’t what they used to be-and that’s okay. What’s not okay is pretending they are.Use the tools available: BIS1 for frail seniors, cystatin C when in doubt, ideal body weight with Cockcroft-Gault when needed. And never let a computer’s default setting be your safety net. Your health is too important for that.

Henriette Barrows
This is the kind of post that makes me want to hug my grandma and then immediately call her pharmacist. I had no idea kidney function dropped this much with age-my dad’s on gabapentin and his doctor just said ‘it’s fine.’ Time to ask for BIS1.