Graves' disease isn't just a thyroid problem-it's your immune system turning against you. Imagine your body sending out the wrong signal, telling your thyroid to produce more hormones than it should. That’s exactly what happens in Graves’ disease. It’s the most common cause of hyperthyroidism, affecting about 1-2% of people, and women are 7 to 8 times more likely to get it than men. Most cases show up between ages 30 and 50. If you’ve been feeling anxious, losing weight despite eating more, or noticing your eyes bulging, it might not just be stress-it could be Graves’.
How Your Immune System Starts the Fire
In a healthy body, the thyroid works like a thermostat. It makes just enough thyroid hormone to keep your metabolism running smoothly. But in Graves’ disease, your immune system produces something called thyroid-stimulating immunoglobulins (TSI). These antibodies act like fake keys, slipping into the thyroid’s TSH receptors and forcing it to overproduce hormones-no matter what your body actually needs.
This isn’t random. Genetics play a role. If someone in your family has Hashimoto’s, type 1 diabetes, or another autoimmune condition, your risk goes up. Smoking doesn’t help either. Smokers are 2 to 3 times more likely to develop Graves’ disease-and if they do, they’re 7 to 8 times more likely to get severe eye complications. The exact trigger isn’t known, but stress, pregnancy, and infections are often linked to when symptoms first appear.
What You’ll Feel-Symptoms Beyond the Basics
People often think hyperthyroidism just means weight loss and a fast heartbeat. But Graves’ hits harder and wider. About 85% of patients feel nervous, jittery, or anxious. Sleep becomes a battle-75% struggle with insomnia. You might have a racing pulse even at rest, hands that shake, or muscles that feel weak, especially in your hips and shoulders. Heat becomes unbearable. You sweat more, even in cool rooms, and you’re constantly hungry, yet still losing weight.
Then there’s the eyes. One in three people with Graves’ develop eye changes. It’s not just dryness or redness. Your eyeballs can bulge forward (called exophthalmos), making it hard to close your eyes fully. You might see double, feel pressure behind your eyes, or notice your vision blurring. In rare but serious cases, the optic nerve gets squeezed, threatening permanent vision loss. About 5% of those with eye symptoms reach this level.
Older adults don’t always act like textbook cases. Instead of anxiety and tremors, they might feel unusually tired, have chest pain, or notice memory lapses. Their heart might race irregularly-atrial fibrillation is common. These subtler signs are often missed, leading to delayed diagnosis.
How Doctors Confirm It
Diagnosing Graves’ isn’t guesswork. It’s a three-step process. First, your doctor checks your symptoms and medical history-especially family autoimmune disease, smoking, and recent stress. Then comes the physical exam: they’ll feel for a swollen thyroid (goiter), check your heart rate (often over 100 bpm), and look at your eyes.
The real proof comes from blood tests. TSH, the brain’s signal to the thyroid, is almost always suppressed-below 0.4 mIU/L. Meanwhile, free T4 and T3 levels are high. But the gold standard? Antibody tests. TSI or TRAb antibodies are present in 90% of cases. If they’re positive, you have Graves’-no further tests needed. If not, doctors may use a radioactive iodine uptake scan. In Graves’, the thyroid soaks up iodine like a sponge, showing a uniform glow. Other causes, like thyroid nodules, show patchy uptake.
Ultrasound is also gaining ground. High blood flow in the thyroid, seen as a "thyroid inferno" on Doppler imaging, can confirm Graves’ without radiation. It’s especially useful for pregnant women or those avoiding radioactive tests.
Three Main Treatment Paths-What Works and What Doesn’t
You have three real options. Each has pros, cons, and timelines. There’s no one-size-fits-all.
1. Antithyroid Medications
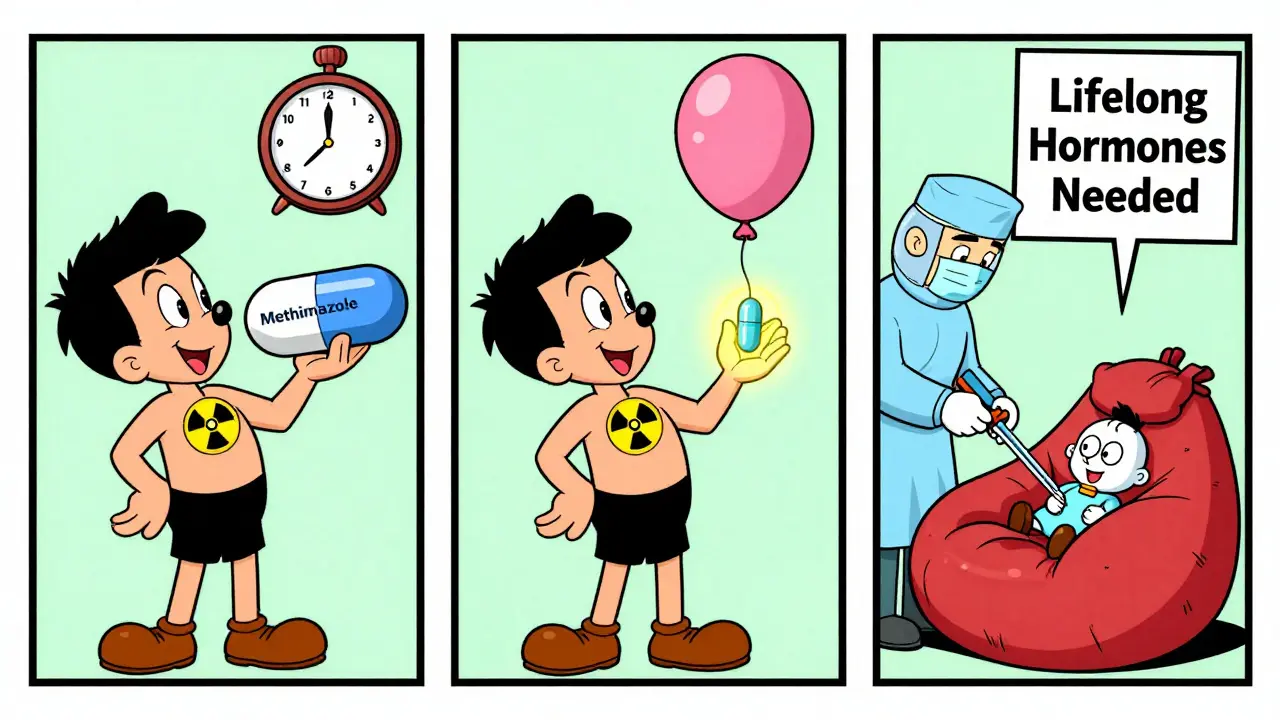
Methimazole is the go-to. It blocks hormone production. Most people start with 10-40 mg daily. It takes 4-8 weeks to bring levels down. Side effects? Rare, but serious. Agranulocytosis-a drop in white blood cells-happens in about 1 in 500 people. If you get a sudden fever or sore throat, stop the drug and get blood work immediately. Propylthiouracil is an alternative, but it carries a higher risk of liver damage.
After 12-18 months, some people go into remission. About 30-50% do. You’re more likely to stay in remission if your goiter is small and your antibody levels drop to zero. But if you stop too early or miss doses, relapse risk jumps by 40-50%. Many patients stay on low-dose methimazole for years-some for life-to avoid flare-ups.
2. Radioactive Iodine (RAI)
This is the most common treatment in the U.S. You swallow a capsule with I-131, a radioactive form of iodine. Your thyroid absorbs it like normal iodine-and the radiation slowly destroys the overactive cells. It’s simple, non-surgical, and effective.
But here’s the catch: 80-90% of people become hypothyroid within a year. That means you’ll need to take levothyroxine for the rest of your life. Dosing starts at about 1.6 mcg per kg of body weight. You’ll need blood tests every 4-6 weeks until your levels stabilize, then every 6-12 months after that.
RAI isn’t for everyone. It’s avoided in pregnant or breastfeeding women. It can also worsen eye disease in active cases. If you have moderate-to-severe Graves’ ophthalmopathy, RAI is usually delayed until eye inflammation is controlled with steroids.
3. Surgery-Thyroidectomy
Removing the thyroid is the most permanent fix. It’s recommended if your goiter is huge and pressing on your windpipe, if you can’t tolerate medications, or if you’re pregnant and can’t use RAI. Success rates are over 95%.
But surgery has risks. There’s a 1-2% chance of damaging the parathyroid glands, which control calcium. That can lead to lifelong calcium supplements. There’s also a 0.5-1% risk of injuring the nerve that controls your voice, causing hoarseness.
After surgery, you’ll need lifelong thyroid hormone replacement. But unlike RAI, you know exactly what’s happening-you’re not waiting months to see if your thyroid shuts down.
Eye Problems? There’s Help
Graves’ eye disease (thyroid eye disease) is separate from the thyroid itself. It’s an autoimmune attack on the fat and muscle behind the eyes. It can get worse even after your thyroid is under control.
For mild cases, selenium supplements (100 mcg twice daily for 6 months) can reduce swelling and discomfort. Lubricating eye drops, sleeping with your head elevated, and quitting smoking help too.
For moderate-to-severe cases, IV steroids are the standard. Methylprednisolone (500 mg weekly for 6 weeks, then 250 mg for another 6 weeks) improves symptoms in 60-70% of people. If that doesn’t work-or if vision is at risk-orbital decompression surgery can relieve pressure and restore eye position.
And now, there’s teprotumumab. This new monoclonal antibody targets the insulin-like growth factor receptor, which drives eye inflammation. In trials, 75-80% of patients saw their bulging eyes shrink significantly. It’s not cheap, and not available everywhere yet-but for those with severe eye disease, it’s a game-changer.
What Patients Say-Real Stories Behind the Stats
On patient forums, you hear the same things over and over. One woman on MyThyroidTeam wrote: "After 3 months on 15 mg methimazole, my heart stopped pounding. I could sleep again. I felt human for the first time in a year."
But others struggle. One man said: "I chose RAI because I didn’t want to take pills forever. Now I’m on levothyroxine, and I still feel tired. No one warned me it would take 6 months to feel normal again."
Eye complications hit hardest. A Reddit user shared: "My eyes stuck out so far I couldn’t close them. Double vision ruined my job. After decompression surgery, I could finally look straight ahead again. It wasn’t perfect-but I got my life back."
One of the biggest regrets? Not being fully informed. Over half of patients surveyed said they wish they’d known more about lifelong medication after RAI or surgery. Many didn’t realize their thyroid could just… stop working.
Living With It-Daily Management Tips
Once you’re diagnosed, your life changes-but not in the way you fear. You can still work, travel, exercise, and live well. Here’s what works:
- Take your meds exactly as prescribed. Missing doses is the #1 reason for relapse.
- Get blood tests regularly. Thyroid levels can drift-even if you feel fine.
- Quit smoking. It’s the single biggest thing you can do to protect your eyes.
- Watch your iodine. Seafood, kelp, and iodized salt aren’t dangerous in normal amounts, but avoid supplements unless your doctor says so.
- Manage stress. Yoga, meditation, or even daily walks can help your immune system settle down.
- Join a support group. Talking to others who’ve been there makes a huge difference.
Most people stabilize within 3-6 months. Quality of life improves dramatically once hormone levels are balanced. But patience matters. Your body took time to go out of balance-it’ll take time to heal.
What’s Next? Research on the Horizon
Science is moving fast. Rituximab, a drug that wipes out B-cells (the immune cells making the bad antibodies), is showing promise in trials for severe eye disease. Early results show 60% response rates after 24 weeks.
Genetic studies have found 12 key genes linked to Graves’-including HLA-DQA1 and CTLA4. That means one day, we might be able to predict who’s at risk before symptoms start.
And researchers are exploring whether gut health, vitamin D levels, or environmental toxins play a role. We’re not there yet-but the pieces are starting to fit together.
Graves’ disease isn’t a death sentence. It’s a chronic condition-with a clear path to control. Whether you choose pills, radiation, or surgery, you’re not alone. And with the right treatment, you can get back to feeling like yourself again.

Windie Wilson
So let me get this straight-I’m supposed to believe my immune system is just *really* bad at its job now? Like, it’s not enough that my body forgets where my keys are, now it’s trying to turn my thyroid into a caffeine factory? Thanks, evolution.