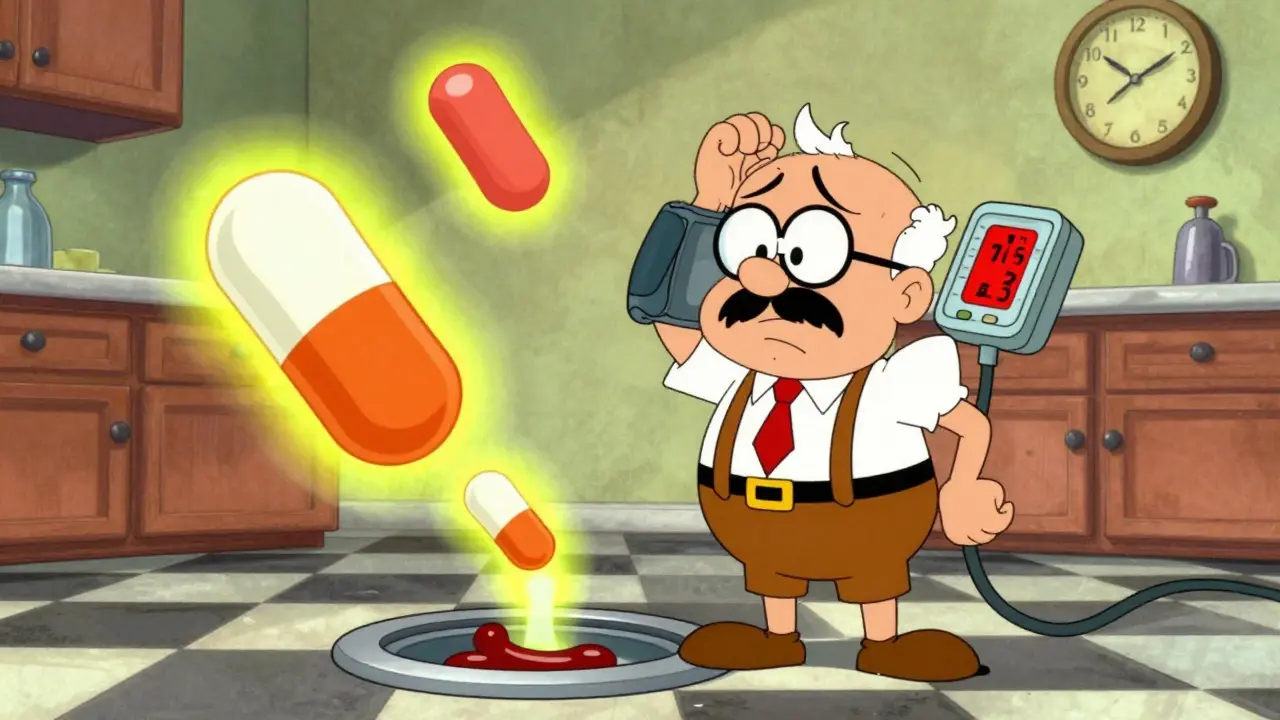
Imagine taking a simple antibiotic for a chest infection, and within two days, your blood pressure plummets so low you faint. This isn’t rare. It happens every day - and it’s entirely preventable. The problem? Combining clarithromycin with common blood pressure medications like nifedipine or amlodipine. The result? A dangerous drop in blood pressure, kidney damage, and sometimes hospitalization.
What’s Actually Happening in Your Body?
Clarithromycin doesn’t just kill bacteria. It also shuts down a key enzyme in your liver called CYP3A4. This enzyme is responsible for breaking down many drugs, including most calcium channel blockers (CCBs). When clarithromycin blocks it, those blood pressure meds don’t get cleared from your system. They build up. And when they do, your blood pressure crashes. Think of it like a clogged drain. The water (the drug) keeps flowing in, but it can’t go out. The pressure builds until something breaks. In this case, it’s your blood pressure. The most dangerous CCBs here are the dihydropyridines - nifedipine, amlodipine, felodipine. Among them, nifedipine is the biggest red flag. Studies show that when clarithromycin is added, nifedipine levels can spike by nearly three times. That’s not a small bump. That’s a medical emergency waiting to happen.Real Cases, Real Consequences
A 76-year-old man in Canada was taking 30 mg of nifedipine daily for high blood pressure. He got a respiratory infection. His doctor prescribed clarithromycin. Within 48 hours, his systolic blood pressure dropped from 130 to 70 mm Hg. He was rushed to the ICU. He needed IV fluids and close monitoring for a full day. Another case: a 72-year-old woman on amlodipine 10 mg daily. After starting clarithromycin, her blood pressure fell to 82 mm Hg systolic. Her heart rate dropped to 48 beats per minute. She was hospitalized. Her doctors later found she was also on a beta-blocker - another drug that slows the heart. That combo made things even worse. These aren’t outliers. A review of U.S. drug safety data from 2010 to 2020 found over 1,800 reported cases of severe hypotension tied to this exact combo. The odds of it happening were nearly four times higher than with other antibiotics.Why Azithromycin Is the Safer Choice
Here’s the good news: there’s a simple fix. Use azithromycin instead. Azithromycin is also a macrolide antibiotic - same class as clarithromycin. But it doesn’t inhibit CYP3A4. It doesn’t interfere with blood pressure meds. It kills the same bacteria. Same dose, same duration. Just safer. A landmark 2013 study tracked nearly 100,000 people on calcium channel blockers who got either clarithromycin or azithromycin. Those on clarithromycin had twice the risk of hospitalization for low blood pressure and kidney injury. Azithromycin? No increased risk. The FDA and Health Canada both warn about this interaction. The FDA even added a black box warning - the strongest possible - to clarithromycin’s label in 2011. Yet, years later, doctors still prescribe it.
Who’s Most at Risk?
This isn’t just about the drugs. It’s about the person. Older adults are the most vulnerable. About 1.2 million Americans over 65 get clarithromycin each year while already on a CCB. That’s 41% of all CYP3A4 substrate drugs they’re taking. The American Geriatrics Society lists clarithromycin as a “potentially inappropriate medication” for seniors on these drugs. People with kidney problems are also at higher risk. If your kidneys aren’t filtering well, drugs stick around longer. Add clarithromycin into the mix, and you’re stacking the deck against yourself. Even if you’re otherwise healthy, don’t assume you’re safe. The interaction can hit fast - within 24 to 72 hours. Symptoms include dizziness, blurred vision, fatigue, confusion, and fainting. If you’re on a CCB and start clarithromycin, check your blood pressure daily. If it drops more than 30 mm Hg from your normal, stop the antibiotic and call your doctor.What You Should Do Now
If you’re on a calcium channel blocker and your doctor prescribes clarithromycin, ask: “Can I use azithromycin instead?” Here’s a quick checklist:- Are you taking nifedipine, amlodipine, felodipine, or nicardipine? If yes, avoid clarithromycin.
- Is your doctor aware you’re on a blood pressure medication? Many aren’t.
- Have you been told to monitor your blood pressure after starting the antibiotic? If not, ask.
- Do you have kidney disease or are over 65? If yes, this combo is especially risky.

What About Other Antibiotics?
Erythromycin is just as dangerous as clarithromycin. It’s another strong CYP3A4 inhibitor. Don’t assume it’s safer. Newer antibiotics like fidaxomicin don’t interfere with CYP3A4. But they’re not used for respiratory infections. So for most cases, azithromycin remains the best alternative. Don’t assume all macrolides are the same. Clarithromycin and erythromycin? High risk. Azithromycin? Safe. Always check.Why Isn’t This Stopped Already?
You’d think hospitals and pharmacies would block this combo automatically. But they don’t. A 2018 study found that only 43% of electronic health record systems had alerts for this interaction. That means most prescribers aren’t warned. Even when alerts exist, they’re often ignored. One study showed that when alerts were active, clarithromycin prescriptions for CCB users dropped by 37%. That’s huge. But most systems still don’t have them. It’s a system failure. Not a medical one. Doctors aren’t evil. They’re overwhelmed. They’re not always aware of the latest data. The science has been clear since 2013. The warnings have been out for over a decade. Yet, this interaction still causes around 8,400 hospitalizations and 320 deaths every year in the U.S. alone.Final Takeaway
This isn’t a theoretical risk. It’s a daily, preventable danger. Clarithromycin and calcium channel blockers don’t mix. The consequences are real, rapid, and sometimes deadly. Azithromycin works just as well - without the risk. There’s no reason to keep using clarithromycin in patients on blood pressure meds. If you’re taking a CCB, check your prescription list. If you see clarithromycin, ask for azithromycin. If you’re prescribing it - stop. Switch. Save a life.Can clarithromycin cause low blood pressure when taken with amlodipine?
Yes. Clarithromycin inhibits the liver enzyme CYP3A4, which breaks down amlodipine. This causes amlodipine levels to rise by up to 60%, leading to dangerously low blood pressure. Symptoms like dizziness, fainting, or confusion can appear within 24-72 hours. A 2015 case report documented a 72-year-old patient whose systolic blood pressure dropped to 82 mm Hg after starting clarithromycin while on amlodipine 10 mg daily.
Is azithromycin safer than clarithromycin with calcium channel blockers?
Yes. Azithromycin does not inhibit CYP3A4, so it doesn’t raise blood levels of calcium channel blockers. A 2013 JAMA study of nearly 200,000 patients found no increase in hypotension or kidney injury with azithromycin, while clarithromycin doubled the risk. Azithromycin is now the recommended alternative for patients on CCBs.
Which calcium channel blockers are most dangerous with clarithromycin?
Dihydropyridine CCBs carry the highest risk: nifedipine > felodipine > amlodipine > nicardipine. Nifedipine is the most dangerous - studies show its levels can increase by 2.8-fold when combined with clarithromycin. Non-dihydropyridines like verapamil and diltiazem also pose a risk, but less so. Always assume any CCB is risky with clarithromycin.
How long does it take for the interaction to cause low blood pressure?
Symptoms usually appear within 24 to 72 hours after starting clarithromycin. In documented cases, patients went from normal blood pressure to critically low levels in under two days. If you’re on a CCB and start clarithromycin, check your blood pressure daily. If it drops more than 30 mm Hg from your baseline, stop the drug and seek help immediately.
Should I stop my calcium channel blocker if I need clarithromycin?
No. Never stop your blood pressure medication without medical advice. Instead, ask your doctor to switch you to azithromycin. Stopping your CCB could cause your blood pressure to spike, which is also dangerous. The solution isn’t stopping one drug - it’s replacing the unsafe one with a safer alternative.
Is this interaction only a problem for older adults?
No. While older adults and those with kidney disease are at higher risk, anyone taking a CCB and clarithromycin is vulnerable. The interaction is based on liver enzyme inhibition, not age. However, older patients are more likely to be on multiple medications, have reduced kidney function, and be more sensitive to blood pressure drops - making them the most common group affected.
Do pharmacists check for this interaction before filling prescriptions?
Some do, but many don’t. Only 43% of electronic health record systems have alerts for this specific interaction. Pharmacists rely on these systems, and without alerts, they may not catch it. Always double-check your own medications. If you’re on a CCB and receive clarithromycin, ask the pharmacist: “Is this safe with my blood pressure pills?”
Can I take clarithromycin if I’m on verapamil or diltiazem?
It’s still risky. Verapamil and diltiazem are not dihydropyridines, but they still interact with clarithromycin. They’re metabolized by CYP3A4 and can cause additive effects on heart rate and blood pressure. The combination may lead to excessive slowing of the heart (bradycardia) and low blood pressure. Azithromycin remains the safest choice regardless of which CCB you’re on.

Lindsey Kidd
OMG I just realized my grandma was on amlodipine and got clarithromycin last winter... she passed out in the kitchen and we thought it was just old age 😭 thank you for posting this. I’m gonna print this out and hand it to her cardiologist tomorrow.