Chronic Fatigue Syndrome isn’t just feeling tired. It’s waking up exhausted after eight hours of sleep, then crashing after brushing your teeth. It’s the kind of fatigue that turns a grocery run into a three-day recovery mission. This isn’t burnout. It’s not laziness. It’s Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) - a real, measurable illness backed by growing clinical evidence and recognized by major health agencies since the 1980s.
What Makes ME/CFS Different From Regular Fatigue?
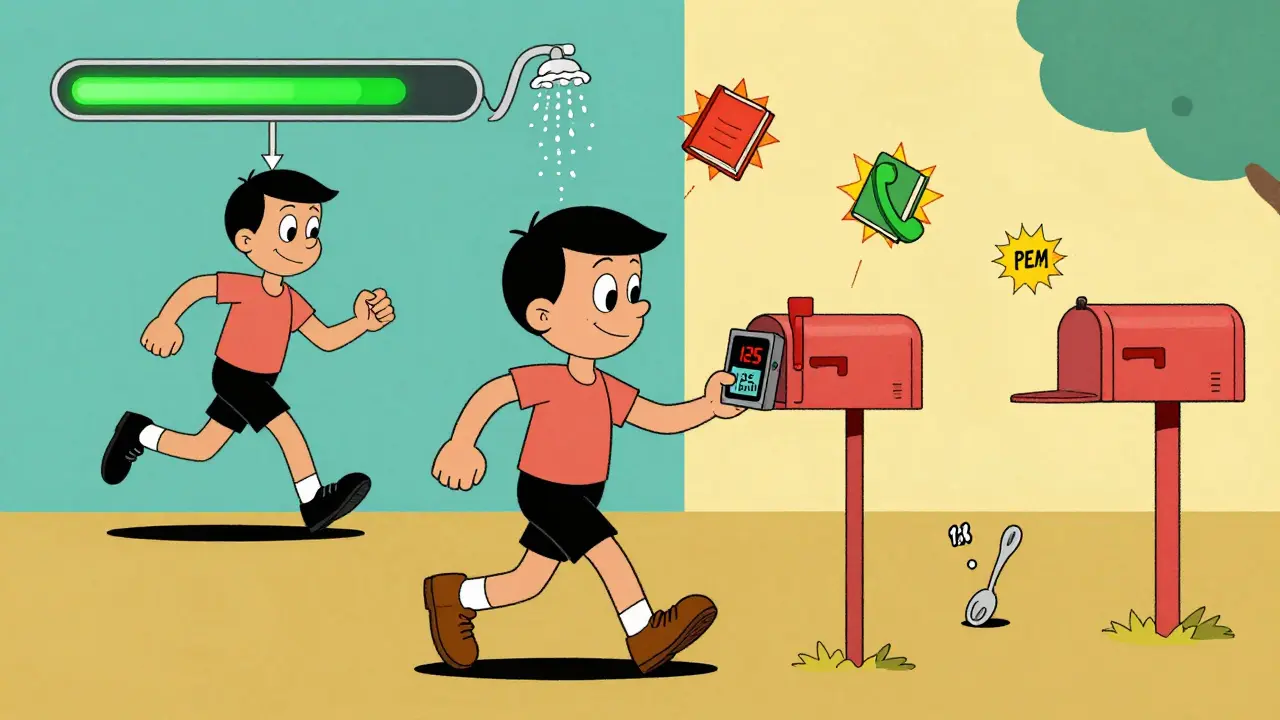
Everyone gets tired. But with ME/CFS, fatigue doesn’t go away with rest. It gets worse with effort - even small ones. That’s called post-exertional malaise, or PEM. It’s the defining feature. After walking to the mailbox, reading a chapter, or even having a long conversation, symptoms can spike hours or days later. People describe it like a battery running out and never recharging. Some wake up with muscle pain they didn’t have the night before. Others can’t think clearly for days after a shower.
The National Institutes of Health and the CDC now confirm ME/CFS is a neurological and immune disorder. Brain scans show reduced connectivity in areas that control attention, memory, and energy regulation. Immune markers like IL-1β and TNF-α rise during PEM episodes. Mitochondria - the energy factories in your cells - produce 28% less ATP. Lactate clears 50% slower than in healthy people. These aren’t theories. These are lab-confirmed abnormalities.
The Three Big Diagnostic Criteria - And Why They Matter
There’s no single blood test for ME/CFS. Diagnosis relies on symptom patterns. Three main frameworks are used today:
- CDC 1988 Criteria: Requires six months of unexplained fatigue plus four of eight symptoms - including sore throat, tender lymph nodes, muscle pain, joint pain, headaches, unrefreshing sleep, and PEM. It’s broad. It catches more people, but also includes false positives.
- IOM 2015 Criteria: Focuses on three core symptoms: severe fatigue, PEM, and unrefreshing sleep. Plus one more: cognitive problems or orthostatic intolerance (dizziness when standing). It’s simpler for doctors to use and has higher specificity. But it misses people whose main issue is PEM without clear brain fog.
- International Consensus Criteria (ICC): Demands PEM as the central symptom, plus problems in at least three of five systems: neurological, immune, gastrointestinal, genitourinary, and energy metabolism. It’s the most precise - 92% specificity - but harder to apply in busy clinics.
A 2022 meta-analysis found the CDC criteria diagnosed 40% more cases than IOM. But the IOM criteria reduced false diagnoses by 25%. The ICC, while most accurate, underdiagnoses because it’s so strict. That’s why many specialists now use a mix - looking for PEM as the non-negotiable symptom, then checking for other patterns.
Why Pacing Is the Only Proven Way to Manage ME/CFS
For decades, doctors told people with ME/CFS to “get more exercise.” That advice was wrong - and harmful. Graded Exercise Therapy (GET) made symptoms worse for 37% of patients in the 2021 STOP ME/CFS trial. Many ended up bedridden.
Pacing - managing energy like a finite resource - is the only strategy backed by consistent results. It’s not about pushing through. It’s about staying within your energy envelope.
Think of it like this: Healthy people have 24-30 “spoons” of energy a day. Someone with ME/CFS might have 12. Every task - showering, cooking, talking - costs spoons. Once you’re out, you crash. Successful patients track their spoons using apps like Fatigue Tracker or simple paper diaries. They aim to stay at 70% of their perceived max capacity. Not 80%. Not 90%. 70%.
Heart rate monitors help. Most people with ME/CFS hit their anaerobic threshold at 120-130 bpm - far below what’s normal. Staying below that reduces PEM by 45%, according to the Workwell Foundation. One patient in Perth, who used a Fitbit to keep her heart rate under 125 during walks, cut her crash days from five per week to one.
It takes time. Most people go through a “boom-bust” cycle at first - overdoing it, crashing, then repeating. It takes 3-4 months of consistent pacing to find a stable baseline. But once they do, 65% of patients at the Bateman Horne Center report 30% symptom improvement within six months.
The Clinical Evidence Is Now Overwhelming
For years, ME/CFS was dismissed as “all in your head.” That’s changed. Here’s what science now confirms:
- Brain Changes: fMRI studies show reduced connectivity in the brainstem and hippocampus - areas tied to alertness and memory. The worse the symptoms, the stronger the signal (r=0.78).
- Immune Dysregulation: Cytokines rise during PEM. IL-1β increases by 42%, TNF-α by 37%. This isn’t inflammation from infection - it’s chronic, low-grade immune activation.
- Autonomic Failure: Heart rate variability drops 35% during tilt-table tests. Your body can’t regulate blood pressure or heart rate properly when standing.
- Metabolic Breakdown: Mitochondria produce less ATP. Lactate builds up faster. The body can’t clear waste products efficiently after even light activity.
These aren’t random findings. They’re replicated across 5 research centers in the U.S. and Europe. In 2023, the Global Burden of Disease study officially reclassified ME/CFS from “idiopathic chronic fatigue” to “neuroimmune disease.” That’s a game-changer for funding, diagnosis, and treatment.
Why Diagnosis Takes So Long - And How to Navigate It
The average person waits 5.2 years to get diagnosed. Sixty-three percent see five or more doctors. Why? Because most doctors aren’t trained to recognize PEM. Many still think it’s anxiety or depression.
Patients report being told:
- “You just need to exercise more.”
- “It’s all in your head.”
- “Try yoga.”
- “Go on vacation.”
That’s not just frustrating - it’s dangerous. Misdiagnosis leads to harmful treatments. The key is to bring documentation. Print out the IOM or ICC criteria. Highlight the PEM section. Bring a symptom diary showing crashes after activity. Mention the 2023 CDC toolkit for providers - it’s now the standard reference.
If your doctor refuses to consider ME/CFS, ask for a referral to a specialist clinic. Centers like Bateman Horne in the U.S. or the ME Association in the UK have protocols. In Australia, the Royal Perth Hospital has a growing ME/CFS clinic. Don’t give up. You’re not imagining this.
What’s Next for ME/CFS Research?
Things are moving faster than ever. The NIH launched a $17.8 million research network in 2022 with five major centers. The FDA now requires objective PEM measurement - via two-day cardiopulmonary exercise tests - for any drug trial. That’s huge. It means treatments must prove they actually reduce crashes, not just “feel better.”
Drugs like Ampligen have shown 35% symptom improvement in trials. Gut microbiome studies are starting in early 2024. Metabolic reprogramming research is underway in Europe. Funding has jumped from $6 million in 2015 to $25 million in 2023 - still low, but growing.
And the stigma? It’s cracking. In 2023, Dr. Anthony Fauci, former head of the NIH, said: “ME/CFS research has entered its most promising phase in 30 years.” That’s not just hope. It’s a turning point.
If you have ME/CFS, you’re not alone. You’re part of a growing community that’s forcing science to listen. And the evidence? It’s no longer on your side. It’s on yours.
Is ME/CFS the same as burnout or depression?
No. Burnout improves with rest and time off. Depression often involves sadness, hopelessness, or loss of interest. ME/CFS is defined by post-exertional malaise - a crash after minimal activity that lasts days. Brain scans, immune markers, and metabolic tests show physical abnormalities not found in depression or burnout. While anxiety or low mood can occur as secondary reactions, they are not the cause.
Can exercise help ME/CFS?
Traditional exercise programs like graded exercise therapy (GET) have been shown to worsen symptoms in 37% of patients. Forced activity triggers PEM and can lead to long-term decline. Pacing - staying within your energy limits - is the only safe and effective approach. Gentle movement like stretching or short walks may be tolerated if kept below your anaerobic threshold (usually 120-130 bpm), but pushing through fatigue is dangerous.
Why is ME/CFS underdiagnosed?
Most doctors aren’t trained to recognize PEM as a core symptom. Many still believe it’s psychological or a result of poor lifestyle. There’s no single blood test, so diagnosis relies on symptom patterns. Patients often face dismissal, misdiagnosis, or blame. A 2023 survey found 82% of patients were told their symptoms were “in their head” before getting a correct diagnosis.
How do I start pacing if I’ve been overdoing it?
Start by cutting your activity level to 50-60% of what you think you can do. Use a heart rate monitor to stay below 120-130 bpm. Track your energy using the spoon theory - assign each task a number of spoons, and cap your daily total at 12-18. Rest before you feel tired. Use apps like Fatigue Tracker or a simple notebook. Give yourself 3-4 months to stabilize. Don’t rush. The goal is to prevent crashes, not to “get back to normal” right away.
Are there any medications for ME/CFS?
There are no FDA-approved drugs yet. Some patients use low-dose naltrexone (LDN) to reduce inflammation, or fludrocortisone for orthostatic intolerance. Ampligen has shown promise in trials but isn’t widely available. Treatments focus on symptom management: sleep aids for unrefreshing sleep, pain relievers for muscle pain, and pacing to prevent crashes. Always consult a specialist - self-treating can worsen symptoms.
How common is ME/CFS?
It affects an estimated 0.2-0.4% of the global population - that’s 17 to 34 million people. In the U.S., 836,000 to 2.5 million people have it, but up to 90% are undiagnosed. Women are diagnosed 2-4 times more often than men, though the reasons aren’t fully understood. It can strike anyone - children, athletes, professionals - at any age.
Final Thoughts: This Is Real. And It’s Getting Better.
If you’ve lived with this, you know how isolating it feels. You’ve been told you’re lazy. You’ve been pushed to do more. You’ve lost jobs, friendships, and parts of yourself. But science is catching up. The evidence is no longer anecdotal. It’s in brain scans, immune markers, and metabolic data. Pacing isn’t a workaround - it’s the foundation of survival. And with more funding, better guidelines, and growing awareness, the future is starting to look less bleak.
You’re not broken. You’re not imagining it. You’re living with a complex, documented illness - and you’re not alone.


Delilah Rose
I’ve been living with this for 11 years and honestly, the pacing thing is the only thing that kept me from ending up in a wheelchair. I used to think if I just pushed harder, I’d get better. Nope. Every time I did, I lost another week. Now I track my heart rate like it’s my job. Stay under 125 bpm, even if it means walking slower than a snail. I don’t care what people say - I’d rather be slow and alive than fast and bedridden. The spoon theory saved my life. I wish I’d known about it sooner.
Also, the part about lactate clearing 50% slower? That’s why I can’t even cook dinner without needing to nap for six hours. It’s not laziness. It’s biochemistry. And it’s real.
People don’t get it until they’ve lived it. I’ve had doctors tell me to ‘try yoga.’ I tried yoga. I cried for three days after. That’s not relaxation. That’s trauma.
But I’m glad science is finally catching up. The brain scans, the immune markers - it’s all there. We’re not making this up. We’re just tired. And broken. And tired of being told to try harder.
Thank you for writing this. I’m not alone anymore.