If you’re paying hundreds of dollars a month for a prescription and it’s stretching your budget thin, you’re not alone. In 2025, nearly 3 in 10 Americans still skip doses or skip filling prescriptions because of cost. But here’s the truth: you don’t have to accept that price tag. There’s often a safer, equally effective, and far cheaper version of your medication available - and you have the right to ask for it.
What Is a Therapeutic Alternative?
A therapeutic alternative isn’t just a generic version of your drug. It’s a different medication - sometimes from the same class, sometimes from a different one - that works just as well for your condition. For example, if you’re on esomeprazole (Nexium) for acid reflux, your doctor might suggest switching to omeprazole, a generic proton pump inhibitor that costs about $15 a month instead of $365. That’s a 96% drop in price.These swaps aren’t random. They’re based on clinical evidence. Studies show that many drugs in the same class - like different statins for cholesterol or different ACE inhibitors for blood pressure - have nearly identical results in real-world use. The American College of Physicians says the key is matching three things: effectiveness, safety, and dosing. If those line up, a switch makes sense.
Therapeutic interchange is different from generic substitution. A generic is the exact same chemical as the brand-name drug. A therapeutic alternative is a different chemical that does the same job. That’s important because sometimes no generic exists - but another drug in a similar class does.
Why Don’t Doctors Always Suggest Cheaper Options?
It’s not that they don’t care. Most doctors want you to take your meds. But here’s the reality: many haven’t been trained to think about cost during a 10-minute visit. They’re focused on symptoms, lab results, and guidelines. They might not know that lisinopril (generic blood pressure med) costs $4 at Walmart while a similar brand like Benicar runs $120. Or that gabapentin can replace pregabalin (Lyrica) for nerve pain at 1/30th the price.One 2023 survey found that 43% of patients said their doctor didn’t even bring up cost-saving options. That doesn’t mean the doctor doesn’t know - it means they’re waiting for you to speak up.
How to Ask for a Lower-Cost Alternative (Step by Step)
You don’t need to be a medical expert. You just need to be clear, prepared, and confident. Here’s how to do it.
- Start with the cost question. During your next appointment, say: “I’m having trouble affording my medication. Is there a cheaper option that works just as well?” That’s all it takes. The American Academy of Family Physicians recommends this exact question because it opens the door without sounding confrontational.
- Do your homework first. Go to GoodRx.com and search your medication. You’ll see prices at nearby pharmacies - and often, cheaper alternatives listed below. For example, if you’re on Eliquis, GoodRx will show warfarin as a possible alternative with a $15 monthly price tag versus $500+. Print or screenshot the page. Bring it with you.
- Name the alternative. Don’t just say, “Is there something cheaper?” Say: “Could I try metformin instead of Jardiance? I saw that metformin works for type 2 diabetes and costs under $5.” Naming the drug shows you’ve done your research and makes it easier for your doctor to say yes.
- Ask about formulary tiers. Ask: “Is this drug on my insurance’s preferred list?” If it’s not, your plan might cover a different drug in the same class at a lower copay. Your pharmacist can check this too.
- Check for patient assistance programs. Many drugmakers offer free or deeply discounted meds if you qualify. Sites like NeedyMeds and RxAssist list programs by drug name. For example, the Jardiance manufacturer offers up to $150/month off for eligible patients.
- Ask for a 90-day supply. Even if the drug isn’t cheaper, getting three months at once often cuts your copay by 25%. That’s an instant savings.

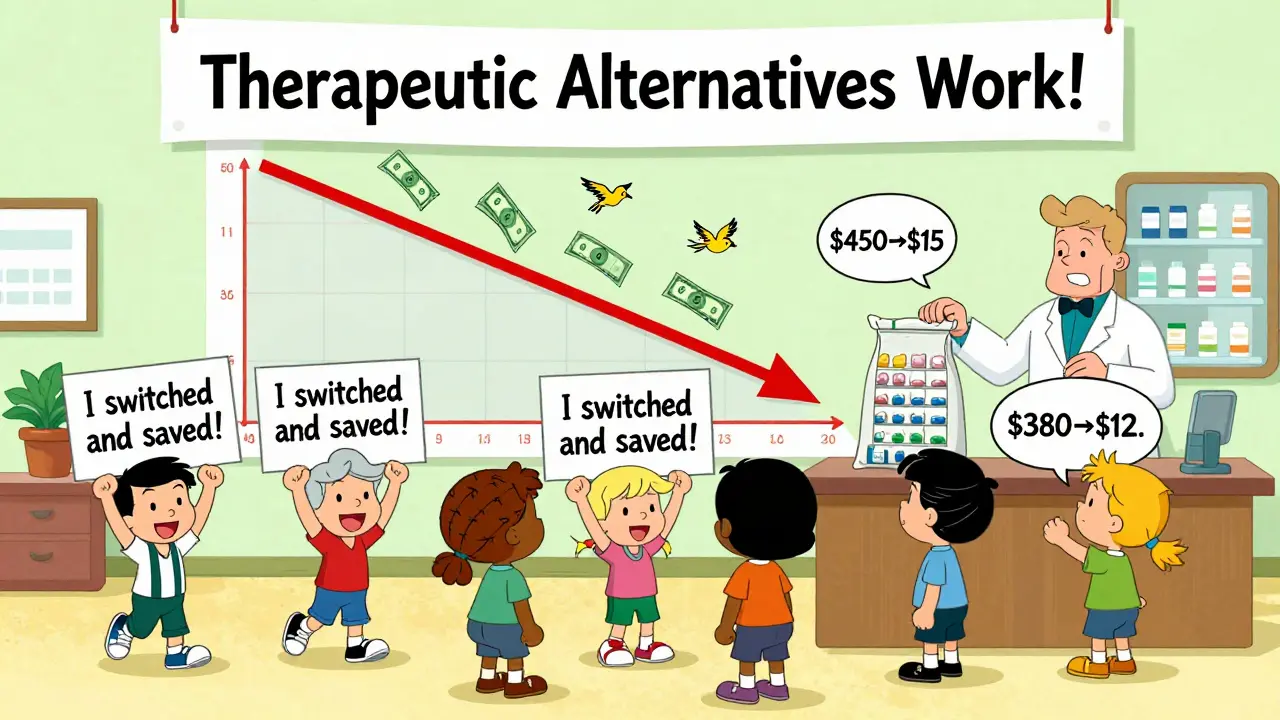
Real Examples of Big Savings
Here are actual swaps that saved people hundreds per month:
- Lyrica (pregabalin) → Gabapentin: $450/month → $15/month for nerve pain
- Crestor (rosuvastatin) → Atorvastatin: $380/month → $12/month for cholesterol
- Xarelto (rivaroxaban) → Warfarin: $500/month → $10/month for blood thinning
- Eliquis (apixaban) → Warfarin: $500/month → $15/month (with regular INR monitoring)
These aren’t outliers. They’re common. The Vanderbilt Medical Center study found that when doctors actively suggested alternatives, patients saved an average of $17.77 per month - which adds up to over $200 a year per person. Multiply that across millions of patients, and you’re talking billions in savings.
When It Doesn’t Work - And What to Do
Not every drug has a good alternative. About 15% of specialty medications - especially biologics for autoimmune diseases or cancer drugs - have no clinically equivalent substitute. In those cases, you’ll need other tools.
If your doctor says no, ask why. Is it because they’re worried about effectiveness? Ask for the evidence. Is it because your insurance won’t cover it? Ask them to file a prior authorization or tiering exception. Medicare and many private insurers must respond to these requests within 72 hours for urgent cases.
Some patients report switching to a cheaper drug and having problems. One person on Reddit switched from Jardiance to metformin and saw their blood sugar spike. That’s why you never switch without medical supervision. But that doesn’t mean you shouldn’t try. It means you need to monitor closely and communicate any changes.
What to Do If Your Doctor Refuses
Doctors are human. They get comfortable with certain prescriptions. If your doctor says no, don’t give up.
- Ask for a referral to a pharmacist who specializes in medication therapy management. Many hospitals and clinics have them.
- Call your insurance company. Ask: “What drugs in this class are covered at Tier 1?” Then bring that list back to your doctor.
- Use the Institute for Clinical Systems Improvement’s free guidelines. They have detailed, evidence-based recommendations for over 125 conditions. Print the page for your condition and hand it to your doctor.
- Consider seeing a second provider. A different doctor might be more open to cost-saving options.
Tools You Can Use Right Now
You don’t need to guess. These tools are free and reliable:
- GoodRx - Compares prices across 70,000+ U.S. pharmacies and lists therapeutic alternatives.
- NeedyMeds - Lists free or low-cost patient assistance programs for over 1,200 drugs.
- RxAssist - Government-backed database of drug discount programs.
- Your pharmacy’s $4 list - Walmart, CVS, and Walgreens all have lists of generic drugs for $4 per 30-day supply. Common ones: lisinopril, metformin, atorvastatin, levothyroxine.
The Bigger Picture
Medication costs aren’t going away. But therapeutic interchange is becoming standard. In 2025, 85% of hospitals and two-thirds of primary care clinics have formal programs to help patients switch to lower-cost options. Electronic health records now flag potential savings at the moment a doctor writes a prescription.
It’s not about cutting corners. It’s about smart care. A 2024 study in JAMA showed that patients who switched to affordable alternatives were more likely to stick with their treatment. That means fewer hospital visits, fewer complications, and better health.
Cost shouldn’t be the reason you skip a pill. You have the power to ask. You have the right to know your options. And you’re not the first person to make this request - millions have done it before you, and they saved hundreds, sometimes thousands, a year.
Next time you get a prescription, ask: “Is there a cheaper option that works just as well?” It might just change your health - and your budget - for good.
Can I ask my pharmacist for a cheaper alternative instead of my doctor?
Yes - but with limits. Pharmacists can suggest generic substitutions and tell you about $4 list drugs or GoodRx coupons. But they can’t change your prescription. Only your doctor can approve a therapeutic alternative. That’s why it’s best to talk to your doctor first. Your pharmacist can help you prepare by showing you price comparisons and listing possible alternatives, which you can then bring to your doctor.
Are therapeutic alternatives as safe as brand-name drugs?
For most people, yes. Therapeutic alternatives are chosen based on clinical trials showing they work just as well with similar side effects. For example, multiple studies have shown that generic atorvastatin and brand-name Crestor have nearly identical effects on cholesterol. But everyone’s body reacts differently. That’s why switching should always be done under medical supervision. If you notice new side effects or worsening symptoms after switching, contact your doctor immediately.
What if my insurance won’t cover the cheaper drug?
Your doctor can file a “tiering exception” request with your insurer. This is a formal appeal asking them to cover a non-preferred drug at a lower cost. Medicare and most private insurers must respond within 72 hours for urgent cases (like if you’re at risk of hospitalization) and within 14 days for standard requests. You’ll need your doctor to explain why the cheaper option won’t work for you - for example, if you had a bad reaction to it before or if your condition is too unstable to switch.
Can I switch to a cheaper drug if I’m on Medicare?
Absolutely. Medicare Part D plans are required to have therapeutic alternatives on their formularies. If your current drug isn’t covered well, ask your doctor to switch you to a preferred drug on your plan’s list. You can also request a formulary exception if your doctor believes the cheaper option won’t work for you. Since 2024, Medicare has required all plans to process these requests faster - within 72 hours for urgent cases.
Do therapeutic alternatives work for chronic conditions like diabetes or high blood pressure?
Yes - and that’s where they make the biggest difference. For conditions requiring lifelong medication, small monthly savings add up fast. Switching from brand-name Jardiance ($450/month) to generic metformin ($5/month) saves $5,400 a year. Studies show patients on affordable meds are more likely to take them consistently, which leads to better long-term outcomes. The American Diabetes Association supports therapeutic interchange for type 2 diabetes when clinical guidelines allow it.

Layla Anna
I switched from Eliquis to warfarin last year and my bank account thanked me 💸... but man, those monthly blood tests? Not fun. Still worth it though.