Methadone QT Risk Calculator
Personal Risk Assessment
This tool helps determine your risk of QT interval prolongation while on methadone treatment based on key factors from clinical guidelines.
Input Your Information
When someone starts methadone for opioid dependence, the focus is usually on reducing cravings, preventing withdrawal, and rebuilding life. But there’s a quiet, invisible risk that doesn’t show up in therapy sessions or urine tests: methadone can mess with your heart’s electrical rhythm. It doesn’t happen to everyone, but when it does, it can be deadly. The good news? We know how to catch it early-and prevent it.
Why Methadone Can Slow Down Your Heart’s Electrical Signal
Methadone works by binding to opioid receptors in the brain, but it doesn’t stop there. It also blocks a specific potassium channel in heart cells called hERG (human ether-a-go-go-related gene). This channel helps reset the heart’s electrical charge after each beat. When it’s blocked, the heart takes longer to recharge. That delay shows up on an ECG as a longer QT interval. The QT interval measures how long it takes the heart’s ventricles to depolarize and repolarize. A normal QTc (corrected for heart rate) is under 430 ms for men and under 450 ms for women. Once it crosses 450 ms in men or 470 ms in women, you’re in the danger zone. At 500 ms or higher, the risk of a deadly arrhythmia called Torsades de Pointes jumps fourfold. This isn’t theoretical-between 2000 and 2022, the FDA recorded 142 confirmed cases of TdP linked to methadone. Many more likely went unreported because sudden deaths in people with opioid use disorder are often written off as overdose.Who’s at the Highest Risk?
Not everyone on methadone needs monthly ECGs. Risk isn’t just about the dose-it’s about the whole picture. The biggest red flags:- Dose above 100 mg/day: The higher the dose, the greater the risk. Studies show patients on over 100 mg/day are nearly four times more likely to have QTc prolongation.
- Female gender: Women have 2.5 times the risk of men, even at the same dose.
- Low potassium or magnesium: If your potassium drops below 3.5 mmol/L or magnesium below 1.5 mg/dL, your heart becomes way more sensitive to methadone’s effects.
- Other QT-prolonging drugs: Mixing methadone with antidepressants like amitriptyline, antipsychotics like haloperidol, or antibiotics like moxifloxacin can push your QT interval into danger territory.
- Heart disease or slow heart rate: If you have heart failure, a past heart attack, or a resting heart rate under 50 bpm, your heart has less reserve to handle the stress.
- Age over 65: Older hearts don’t recover as quickly from electrical disruptions.
- Drug interactions: Medications that block the CYP3A4 liver enzyme-like fluconazole, voriconazole, or fluvoxamine-can spike methadone levels by up to 50%, turning a safe dose into a dangerous one.
And here’s something many don’t realize: about half of people on methadone have sleep apnea. That means your oxygen drops at night, stressing your heart even more. It’s not just the drug-it’s the combo.
When and How Often Should You Get an ECG?
The key is risk-based monitoring, not blanket screening. Here’s what the guidelines say:- Baseline ECG: Get one before you start methadone-or within the first week. This gives you a personal baseline. Don’t skip this, even if you feel fine.
- Repeat at steady state: Methadone builds up slowly. Wait 2 to 4 weeks after starting or changing your dose before testing again. That’s when levels stabilize.
After that, frequency depends on your risk level:
- Low risk: QTc under 450 ms (men) or 470 ms (women), no other risk factors. Get an ECG every 6 months.
- Moderate risk: QTc between 450-480 ms (men) or 470-500 ms (women), or one or two other risk factors. Monitor every 3 months.
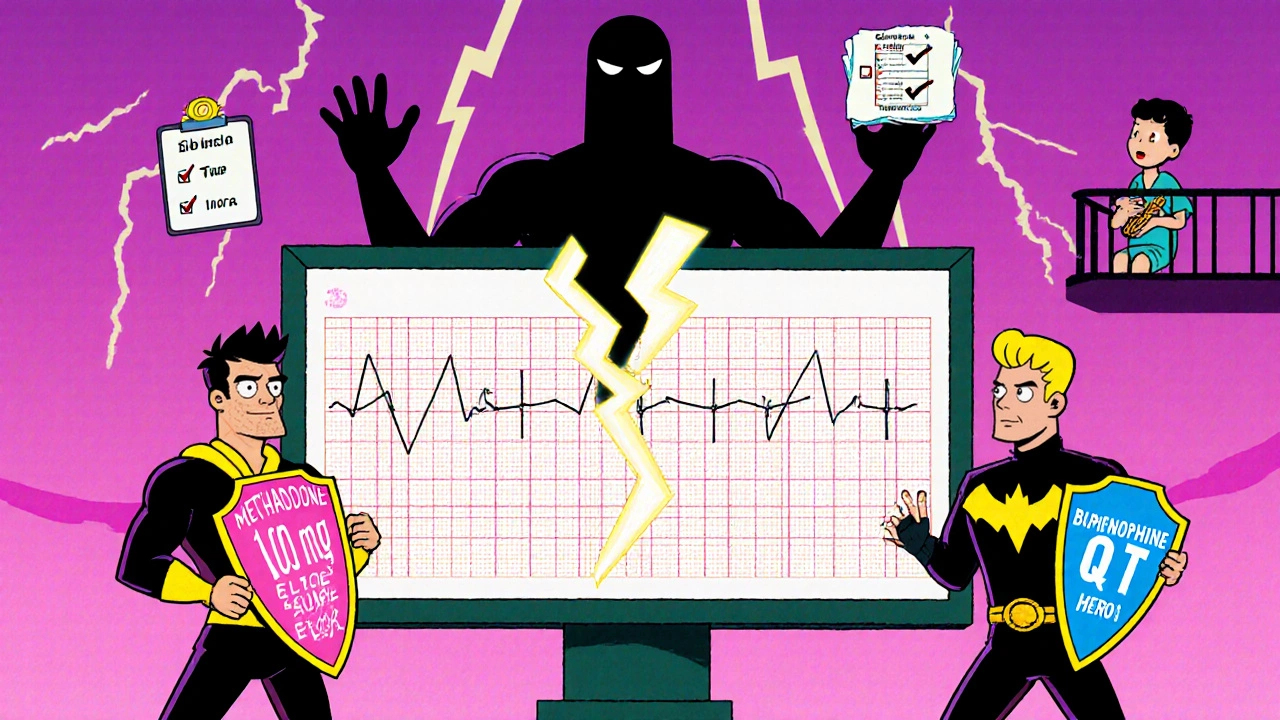
- High risk: QTc over 480 ms (men) or 500 ms (women), or three or more risk factors. Get an ECG every month. Consider lowering your dose or switching to buprenorphine, which has a much lower risk of QT prolongation.
A 2023 study in JAMA Internal Medicine showed that clinics with structured ECG monitoring had a 67% lower rate of serious cardiac events than those that didn’t. That’s not just a trend-it’s life-saving.
What to Do If Your QTc Is Too Long
If your QTc is above 500 ms, or if it jumped more than 60 ms from your baseline, don’t wait. Take action:- Check your electrolytes: Get a blood test for potassium and magnesium. If they’re low, correct them. A simple oral supplement can make a big difference.
- Review all your meds: Go through every prescription, OTC drug, and supplement with your doctor. Stop anything that prolongs QT if possible.
- Reduce your methadone dose: Even a 10-20% drop can bring QTc back down. Don’t panic-this isn’t failure. It’s safety.
- Get a cardiology consult: Especially if you have symptoms like dizziness, fainting, or palpitations.
- Consider switching to buprenorphine: It’s just as effective for most people at managing opioid dependence, with far less cardiac risk.
One real-world study in Geneva found that nearly 9% of patients on methadone had QTc over 500 ms. Almost all of them had at least two risk factors. That’s not bad luck-it’s a system failure. If monitoring had been routine, many of those cases could’ve been caught earlier.
Why So Many Clinics Are Still Getting This Wrong
Despite clear guidelines from SAMHSA, the American Heart Association, and the FDA, many methadone clinics still don’t have standardized ECG protocols. A 2022 Reddit survey of 142 people in recovery found that 68% said their clinic didn’t consistently monitor QT intervals. Some didn’t do it at all. Others did it only if you asked.Patients who got regular monitoring reported feeling safer. Eighty-two percent said they trusted their treatment more. Only 47% of those without monitoring felt the same. It’s not just about data-it’s about peace of mind.
There’s also a stubborn myth: “If I don’t feel anything, it’s fine.” But Torsades de Pointes often strikes without warning. No chest pain. No dizziness. Just a sudden, silent stop. That’s why we monitor before it’s too late.
What You Can Do Right Now
If you’re on methadone:- Ask for your last ECG result. If you don’t have one, request it now.
- Know your QTc number. Don’t let your doctor just say “it’s normal.” Ask for the exact number.
- Keep track of your potassium. Eat bananas, potatoes, spinach, or ask about supplements if your levels are low.
- Tell your prescriber about every other medication-even herbal ones.
- If you’ve had fainting spells, irregular heartbeats, or unexplained dizziness, speak up. Don’t assume it’s just “the methadone.”
If you’re a provider:
- Make baseline ECG part of your intake checklist.
- Use risk stratification-not one-size-fits-all.
- Track QTc over time. A single normal reading doesn’t mean it stays normal.
- Have a plan for when QTc rises. Don’t wait for a crisis.
Methadone saves lives. But like all powerful tools, it needs careful handling. The goal isn’t to scare people away from treatment-it’s to make sure that treatment doesn’t cost them their heart.
Can methadone cause sudden cardiac death even if I feel fine?
Yes. Methadone can trigger Torsades de Pointes-a dangerous heart rhythm-without warning symptoms. Many people who die from this don’t have chest pain or dizziness beforehand. That’s why monitoring QTc with ECGs is critical, even if you feel perfectly healthy.
Is buprenorphine safer than methadone for the heart?
Yes. Buprenorphine has a significantly lower risk of QT prolongation compared to methadone. Studies show it rarely causes clinically significant QTc changes, even at high doses. For patients with multiple risk factors or a history of prolonged QT, switching to buprenorphine is often the safest choice without losing treatment effectiveness.
How often should I get an ECG if I’m on methadone?
It depends on your risk. Low-risk patients (no other risk factors, QTc under 450 ms for men or 470 ms for women) need one every 6 months. Moderate-risk patients (one or two risk factors, QTc in the borderline range) should be monitored every 3 months. High-risk patients (QTc over 480 ms for men or 500 ms for women, or three or more risk factors) need monthly ECGs and possible dose adjustment.
Can low potassium make methadone more dangerous for my heart?
Absolutely. Low potassium (below 3.5 mmol/L) makes your heart much more sensitive to methadone’s effects on the QT interval. Even a mild drop can turn a safe dose into a risky one. Regular blood tests and eating potassium-rich foods like bananas, sweet potatoes, and spinach can help prevent this.
Should I stop methadone if my QTc is prolonged?
Not necessarily. The first step is to correct electrolytes, review other medications, and reduce the methadone dose slightly. Many people see their QTc improve with these changes. Stopping methadone abruptly can lead to withdrawal and relapse. Work with your provider to find a safer balance-not an all-or-nothing choice.
Why do some clinics not monitor QTc regularly?
Many clinics lack resources, standardized protocols, or awareness. Some providers still believe that if the patient feels fine, there’s no risk. Others don’t know the guidelines. But research shows structured monitoring cuts cardiac events by two-thirds. It’s not optional-it’s essential care.
Can sleep apnea increase the risk of heart problems on methadone?
Yes. About half of people on methadone maintenance have sleep apnea. During apnea episodes, oxygen levels drop, stressing the heart and increasing the chance of arrhythmias. If you snore loudly, wake up gasping, or feel exhausted during the day, ask for a sleep study. Treating sleep apnea can reduce cardiac risk significantly.
What if I’m on a low dose of methadone, like 40 mg/day?
Even low doses can cause QT prolongation in high-risk people. If you’re female, over 65, have heart disease, low potassium, or take other QT-prolonging drugs, you still need a baseline ECG. Dose alone doesn’t determine risk-it’s the combination of factors.

Dion Hetemi
Let’s be real - this is the kind of post that should be printed and taped to every methadone clinic wall. I’ve seen too many people get handed a script and told to ‘just show up’ while their QT interval creeps up like a slow-motion car crash. The FDA stats? Real. The 142 confirmed TdP cases? That’s not a number - that’s 142 families who got a call they never saw coming. And half of these folks probably had sleep apnea they never got checked for. It’s not just about the drug. It’s about the whole damn system ignoring the quiet killers.
Someone needs to make a viral TikTok of a cardiologist explaining this to a 22-year-old who thinks ‘I feel fine’ means ‘I’m safe.’