Agranulocytosis Risk Assessment Tool
Medication & Monitoring Assessment
Risk Assessment Results
Agranulocytosis is a life‑threatening drop in white blood cells, specifically neutrophils, where the absolute neutrophil count (ANC) falls below 100 cells/µL. When drugs cause this collapse, clinicians face a steep rise in severe infections and a narrow window for intervention.
Why Medication‑Induced medication-induced agranulocytosis Matters
About 70% of agranulocytosis cases stem from drugs, according to VisualDx (2023). Mortality can hit 20% without rapid treatment, but timely drug discontinuation and vigilant monitoring can push survival above 95% (JCO 2021). The stakes are high because a single infection in this setting can become fulminant, leading to sepsis, organ failure, or death.
Who’s at Risk? High‑Risk Drug Classes
Over 200 medications across 15 classes have been linked to agranulocytosis. The most notorious are:
- Clozapine - antipsychotic with an absolute risk of ~0.8% (FDA 2022).
- Propylthiouracil - antithyroid drug, incidence 0.3-0.5 per 10,000 patient‑years (Endocrine Society 2020).
- Trimethoprim‑sulfamethoxazole - antibiotic, relative risk 15.8 versus non‑users (JAMA Intern Med 2019).
- Dipyrone (metamizole) - NSAID‑type analgesic, incidence ~1.2 per 10,000 patient‑years.
Other agents like carbamazepine, ticlopidine, and certain biologics sit in moderate‑risk tiers and still demand periodic blood checks.
How the Drugs Attack Neutrophils
Two main mechanisms drive the decline:
- Immune‑mediated destruction - about 60% of cases. The drug binds to neutrophil surface proteins, prompting the immune system to generate antibodies that destroy the cells.
- Direct bone‑marrow suppression - roughly 40% of cases. Cytotoxic effects blunt granulocyte precursor production.
Understanding the pathway helps clinicians anticipate the speed of onset: immune reactions can appear within days, whereas marrow suppression may need weeks to months.
Clinical Red Flags: When to Suspect Agranulocytosis
Key symptoms often mimic benign infections, which leads to delays:
- Fever >38.3 °C (often the first sign).
- Sore throat, oral ulcers, or gingivitis.
- Unexplained fatigue or malaise.
According to Dr. Sedhai (NIH StatPearls 2023), fever in a patient on a high‑risk drug with ANC <500 µL is a medical emergency requiring immediate broad‑spectrum antibiotics.
Monitoring Protocols: Frequency and Thresholds
Guidelines from the American Society of Hematology (2022) and the European Hematology Association (2021) converge on a tiered monitoring schedule.
| Drug | Incidence (per 10,000) | Monitoring Frequency | Intervention Threshold (ANC) |
|---|---|---|---|
| Clozapine | 7.7 | Weekly (first 6 mo), bi‑weekly (next 6 mo), monthly thereafter | <1,000 µL or 50 % drop from baseline |
| Propylthiouracil | 0.3-0.5 | Every 4 weeks for 6 mo, then every 3 mo | <500 µL |
| Trimethoprim‑sulfamethoxazole | 1.2 (high‑risk groups) | Baseline CBC, then if therapy >2 weeks repeat | <500 µL |
| Dipyrone | 1.2 | Baseline, then every 6 weeks | <500 µL |
Both the ASH and EHA now recommend acting when ANC drops below 1,000 µL because data show a 78% sensitivity for predicting serious infection at that level.
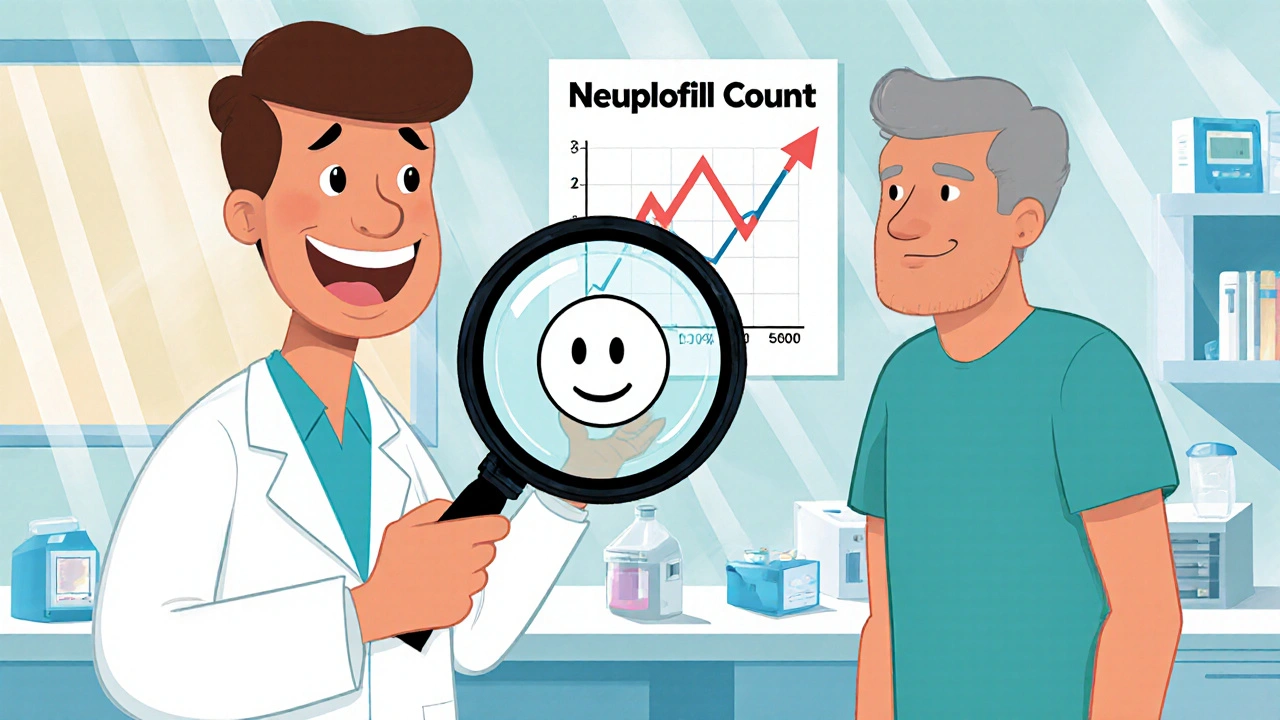
Step‑by‑Step Management When ANC Falls
- Immediately stop the suspected drug.
- Obtain a repeat CBC within 24 hours to confirm the trend.
- Start empiric broad‑spectrum antibiotics covering Pseudomonas aeruginosa (IDSA 2022 recommendation).
- Consider granulocyte‑colony stimulating factor (G‑CSF) if ANC <100 µL or infection is severe.
- Monitor daily CBCs until ANC rises above 500 µL, then weekly until stable.
- Document the adverse event in the patient’s electronic health record and report to the FDA’s MedWatch system.
Recovery typically occurs within 1-3 weeks after drug withdrawal, but individual timelines vary.
Patient Education: Empowering Early Detection
Patients should receive a simple checklist:
- Take temperature twice daily - seek care if >38.3 °C.
- Report mouth sores, sore throat, or new fatigue immediately.
- Never skip scheduled CBC appointments.
- Know the name of the high‑risk medication and its monitoring schedule.
Studies show that patients with strict monitoring feel 92% “more secure” (Schizophrenia Research 2021) and are far less likely to develop severe infection.
Emerging Tools: From Point‑of‑Care Tests to Genomics
Fast bedside ANC devices, such as the Hemocue WBC DIFF (FDA cleared 2022), give results in 5 minutes and have lifted adherence rates by 31% in multicenter trials (Blood Advances 2022). On the genetics front, the HLA‑DQB1*05:02 assay predicts a 14‑fold higher risk for clozapine‑induced agranulocytosis (NEJM Evidence 2023). Incorporating such tests before starting high‑risk drugs could shift the risk‑benefit balance dramatically.
Barriers to Effective Monitoring
Real‑world data expose gaps:
- Only 68% of US clozapine prescribers meet weekly CBC requirements during the first 18 weeks (Psychiatric Services 2020).
- Rural clinics lack on‑site labs; 38% of patients experience delays (AJMC 2021).
- Patient non‑adherence reaches 22.7% for clozapine monitoring (JAMA Net Open 2020).
Solutions include tele‑lab services, mobile phlebotomy, and AI‑driven EHR alerts that have cut missed cases by 47% in a 12‑hospital study (JAMIA 2022).
Future Directions: Toward Safer Prescribing
By 2028, the Personalized Medicine Coalition predicts 40% of high‑risk drugs will require pre‑treatment genetic screening. Regulatory bodies like the FDA are already integrating pharmacogenomic warnings into drug labels. Meanwhile, the global agranulocytosis diagnostics market is projected to hit $2.3 billion in 2022 and grow 6.8% annually, reflecting rising demand for reliable tests.
Clinicians who combine vigilant monitoring, patient education, and emerging predictive tools will dramatically lower infection‑related mortality and keep patients on therapies that might otherwise be abandoned.
Quick Takeaways
- Agranulocytosis caused by drugs is a medical emergency-mortality drops from 20% to <5% with rapid action.
- High‑risk drugs include clozapine, propylthiouracil, trimethoprim‑sulfamethoxazole, and dipyrone.
- Act when ANC falls <1,000 µL; stop the drug, start broad‑spectrum antibiotics, and consider G‑CSF.
- Weekly CBCs for clozapine, then tapering frequency; similar tiered schedules apply to other agents.
- Point‑of‑care tests and HLA‑typing are reshaping early detection and prevention.
Frequently Asked Questions
What ANC level defines agranulocytosis?
Agranulocytosis is defined by an absolute neutrophil count (ANC) of less than 100 cells per microliter of blood.
Which medications carry the highest risk?
Clozapine has the highest documented risk (~0.8%). Other notable agents are propylthiouracil, trimethoprim‑sulfamethoxazole, and dipyrone.
How soon after starting a drug can agranulocytosis appear?
Onset ranges from a few days (immune‑mediated) to several months (bone‑marrow suppression). Most cases emerge within the first 1-3 months.
What immediate steps should be taken if ANC drops below 1,000 µL?
Stop the suspected drug, repeat ANC within 24 hours, start empiric broad‑spectrum antibiotics (including coverage for Pseudomonas), consider G‑CSF, and monitor daily until recovery.
Can genetic testing prevent drug‑induced agranulocytosis?
Yes. The HLA‑DQB1*05:02 assay predicts a >14‑fold increased risk for clozapine‑related agranulocytosis, allowing clinicians to choose alternative therapies or intensify monitoring.

asha aurell
A simple blood count can save lives, yet many still ignore basic monitoring.