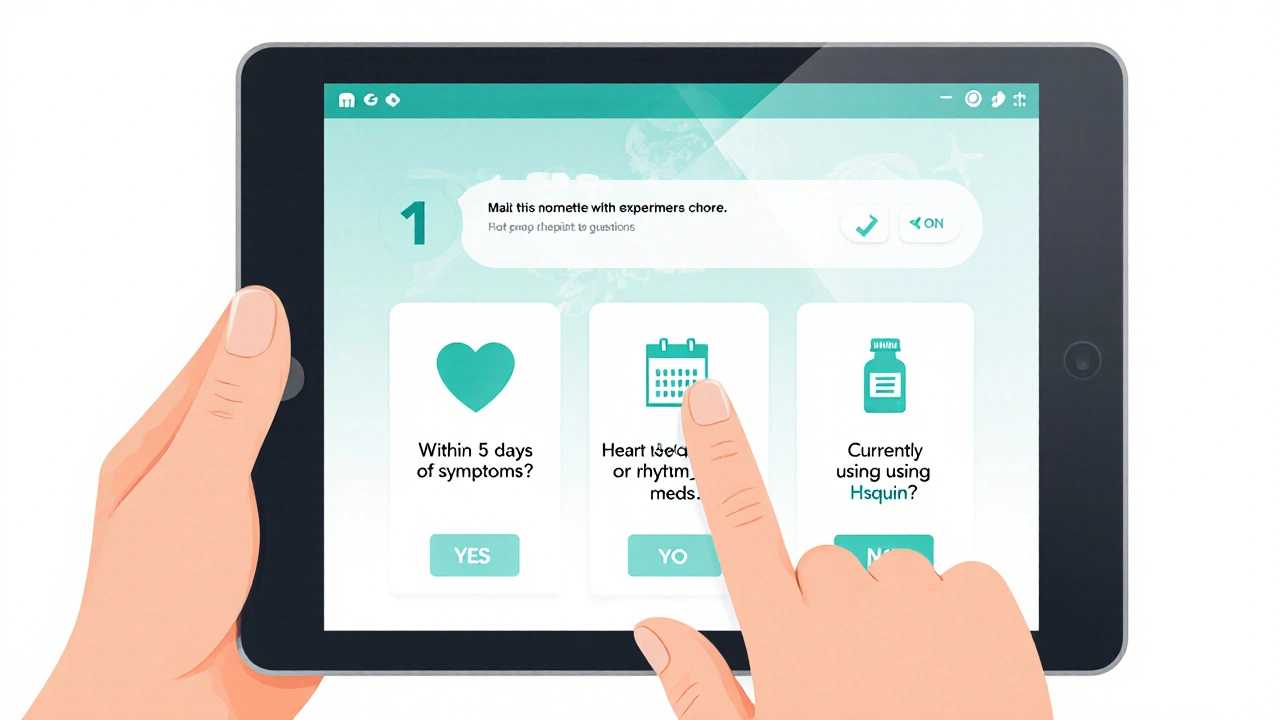
COVID-19 Treatment Decision Helper
Use this tool to determine the most suitable antiviral treatment for your situation based on key factors.
Your recommended treatment will appear here after answering the questions above.
Key Takeaways
- Hsquin (hydroxychloroquine) is approved for malaria and autoimmune diseases, not for COVID‑19.
- Antiviral alternatives such as Paxlovid, Molnupiravir, and Remdesivir have stronger clinical evidence against COVID‑19.
- Safety profiles differ: Hsquin can cause cardiac arrhythmia, while ivermectin’s main risk is neurotoxicity at high doses.
- Regulatory status matters - FDA and WHO endorse only a handful of antivirals for COVID‑19 treatment.
- Choosing a therapy should balance efficacy, side‑effects, drug interactions, and local approval.
When weighing treatment options, Hsquin is a brand name for hydroxychloroquine, a 4‑aminoquinoline originally created to fight malaria and later repurposed for autoimmune disorders like lupus and rheumatoid arthritis. The drug resurfaced in headlines during the early COVID‑19 pandemic, but scientific consensus now places it far behind newer antivirals. This guide lines up Hsquin against the most widely discussed alternatives, breaking down how each works, what the data say, and where they stand with regulators.
Why Hsquin Isn’t the First Choice for COVID‑19 Anymore
Hydroxychloroquine showed modest antiviral activity in isolated cell studies, yet large‑scale trials (RECOVERY, SOLIDARITY) found no mortality benefit for hospitalized patients. Its half‑life stretches beyond a month, leading to prolonged exposure and a higher chance of side‑effects such as QT‑prolongation, retinopathy, and hypoglycemia. Because the drug’s therapeutic window is narrow, clinicians now reserve it for proven indications - malaria prophylaxis, systemic lupus erythematosus, and rheumatoid arthritis.
Alternative Treatments: The Current Contenders
The landscape of COVID‑19 therapeutics has shifted dramatically. Below are the eight most referenced alternatives, each introduced with schema markup for easy knowledge‑graph mapping.
Ivermectin is an antiparasitic approved for treating river blindness and strongyloidiasis. It gained off‑label attention during the pandemic, but well‑designed trials have not demonstrated consistent clinical benefit.
Remdesivir is a nucleotide analogue that inhibits viral RNA‑dependent RNA polymerase. The FDA granted Emergency Use Authorization (EUA) for hospitalized COVID‑19 patients, and later full approval for specific indications.
Doxycycline is a broad‑spectrum tetracycline antibiotic. Its anti‑inflammatory properties led to experimental combo regimens, yet robust data for monotherapy are lacking.
Azithromycin is a macrolide antibiotic often paired with hydroxychloroquine early in the pandemic. Subsequent studies show no added benefit and raise concerns about cardiac toxicity when combined.
Molnupiravir is an oral ribonucleoside analogue that induces lethal mutagenesis in SARS‑CoV‑2. Clinical trials reported about a 30% reduction in hospitalisation when given within five days of symptom onset.
Paxlovid (nirmatrelvir+ritonavir) is a protease inhibitor combo that earned full FDA approval for early outpatient treatment, showing an 89% drop in hospitalisation risk.
Favipiravir is a viral RNA polymerase inhibitor used for influenza in Japan. It has been studied in several countries for COVID‑19, but results remain mixed and it lacks major regulatory endorsement outside of limited settings.
Side‑Effect Profiles: Safety First
Understanding adverse events is essential, especially for patients on multiple meds. Below is a quick safety snapshot:
- Hsquin (hydroxychloroquine): Cardiac arrhythmias (QT prolongation), retinal toxicity (vision changes after long‑term use), hypoglycemia, dermatologic reactions.
- Ivermectin: Neurological symptoms (tremor, seizures) at doses above approved levels, mild GI upset.
- Remdesivir: Elevated liver enzymes, infusion‑related hypersensitivity, possible kidney function impact.
- Doxycycline: Photosensitivity, esophageal irritation, altered gut flora.
- Azithromycin: QT prolongation (especially with other QT‑prolonging drugs), GI upset.
- Molnupiravir: Mild diarrhea, dizziness; theoretical mutagenic concerns, though not observed clinically.
- Paxlovid: Strong drug‑drug interactions via CYP3A inhibition, bitter taste, occasional liver enzyme rise.
- Favipiravir: Hyperuricemia, liver enzyme elevation, teratogenic potential.
Regulatory Landscape (2025)
Regulators worldwide have drawn clear lines around which drugs are acceptable for COVID‑19 therapy:
| Drug | Primary Indication | Mechanism | Clinical Efficacy (COVID‑19) | Safety Concerns | Regulatory Status (USA) |
|---|---|---|---|---|---|
| Hsquin (Hydroxychloroquine) | Malaria, lupus, rheumatoid arthritis | Inhibits parasite heme polymerisation; modulates endosomal pH | No mortality benefit; modest symptom relief in early mild cases (inconsistent) | QT prolongation, retinal toxicity | Approved for malaria & autoimmune disease; no EUA for COVID‑19 |
| Paxlovid | Early COVID‑19 (outpatient) | Protease inhibition (nirmatrelvir) + CYP3A boost (ritonavir) | 89% reduction in hospitalisation when started ≤5days | Drug‑drug interactions, bitter taste | Full FDA approval (2022); WHO recommendation |
| Molnupiravir | Early COVID‑19 (outpatient) | Lethal mutagenesis of viral RNA | ≈30% reduction in hospitalisation | Potential mutagenicity (theoretical), mild GI upset | EUA (2022) - not yet full approval in US |
| Remdesivir | Hospitalised COVID‑19 | RNA‑polymerase chain termination | Reduced median recovery time; modest mortality impact | Liver enzyme elevation, infusion reactions | FDA full approval (2020); WHO conditional recommendation |
| Ivermectin | Parasitic infections | Glutamate‑gated chloride channel agonist | No reproducible benefit in rigorous trials | Neurotoxicity at high doses | Not authorised for COVID‑19 (FDA) |
| Doxycycline | Bacterial infections, acne | Protein synthesis inhibition (30S ribosomal subunit) | Limited data; used only in combination regimens | Photosensitivity, GI upset | Approved for bacterial use; no COVID‑19 indication |
| Azithromycin | Bacterial infections, atypical pneumonia | Inhibits 50S ribosomal subunit | No added benefit when combined with Hsquin; increased cardiac risk | QT prolongation, GI issues | Approved for bacterial use only |
| Favipiravir | Influenza (Japan); experimental COVID‑19 | RNA‑dependent RNA polymerase inhibition | Mixed outcomes; not WHO‑recommended | Hyperuricemia, teratogenic risk | Not FDA‑approved for COVID‑19 |
How to Choose the Right Option for You
Deciding which drug fits your situation hinges on three practical questions:
- Am I early in the disease course? Oral antivirals (Paxlovid, Molnupiravir) work best within the first five days of symptoms.
- Do I have contraindications or drug interactions? For example, Paxlovid’s ritonavir component can boost levels of many heart‑burn meds and statins, requiring dose adjustments.
- What does my local health authority endorse? In Australia, the Therapeutic Goods Administration (TGA) follows FDA/EUA guidance, meaning Paxlovid and Remdesivir are the primary options.
If you’re managing a chronic autoimmune condition, continue your prescribed Hsquin under rheumatology supervision. For an acute COVID‑19 infection, shift to an approved antiviral as soon as you’re eligible.

Practical Tips for Clinicians and Patients
- Verify dosing schedules: Paxlovid requires a 5‑day course (300mg nirmatrelvir + 100mg ritonavir twice daily).
- Monitor cardiac health: Obtain a baseline ECG before prescribing Hsquin or Azithromycin, especially in patients with existing heart disease.
- Watch for drug-drug interactions: Use a trusted interaction checker when adding ritonavir‑boosted regimens.
- Educate patients on warning signs: palpitations, visual changes, or sudden shortness of breath should trigger immediate medical review.
- Document the indication clearly in the medical record to avoid off‑label liability.
Frequently Asked Questions
Can Hsquin prevent COVID‑19 infection?
No. Large randomized trials have shown that hydroxychloroquine does not reduce the risk of acquiring SARS‑CoV‑2 or developing severe disease.
Is Paxlovid safe for people on blood thinners?
Paxlovid can increase levels of some anticoagulants (e.g., warfarin). Close INR monitoring and possible dose adjustment are recommended.
What’s the difference between Molnupiravir and Remdesivir?
Molnupiravir is an oral pill that induces viral mutagenesis, while Remdesivir is an IV infusion that halts viral RNA synthesis. Molnupiravir is used early outpatient, Remdesivir is for hospitalized patients.
Why do some sources still recommend ivermectin?
Misinformation and anecdotal reports keep ivermectin in public discourse, but peer‑reviewed data have not confirmed a therapeutic effect against COVID‑19.
Can I combine Hsquin with azithromycin safely?
Both drugs can prolong the QT interval, raising the risk of dangerous heart rhythms. Combining them is generally discouraged unless under strict cardiac monitoring.
Next Steps for Readers
If you’re a patient currently taking Hsquin for lupus, talk to your rheumatologist before stopping-it may take weeks for the drug to clear from your system. If you’ve just tested positive for COVID‑19 and are within five days of symptoms, contact your primary care provider about eligibility for Paxlovid or Molnupiravir.
Health professionals should review the latest TGA and CDC guidelines before prescribing, document the specific indication, and schedule follow‑up labs (electrolytes, liver function, ECG) as appropriate.
Staying informed and matching the right drug to the right scenario saves lives, reduces side‑effects, and keeps the healthcare system running smoothly.

Debbie Frapp
Taking a step back, it's useful to remember that the pandemic taught us how quickly treatment guidelines can evolve, and staying updated is vital for anyone managing COVID‑19 risks.