When you're managing type 2 diabetes and your doctor suggests a sulfonylurea, it’s easy to assume they’re all the same. After all, they all lower blood sugar by pushing your pancreas to make more insulin. But here’s the truth: not all sulfonylureas are created equal. Some carry a much higher risk of dangerous low blood sugar - especially in older adults, people with kidney issues, or those who skip meals. The difference isn’t small. It’s the difference between going to the ER and staying safe at home.
Why the Choice Matters More Than You Think
Sulfonylureas have been around since the 1950s. They’re cheap, effective, and still used by millions. In 2022, about 15% of U.S. adults with type 2 diabetes were taking one. But here’s the catch: while they lower A1C by 1.5% to 2%, they also cause low blood sugar - sometimes badly. A 2017 study in Diabetes Care found that long-acting sulfonylureas like glyburide caused nearly three times more severe hypoglycemia than short-acting ones like glipizide. That’s not a typo. Three times. The reason? It’s all about how long the drug stays active in your body. Glyburide and glimepiride stick around for hours, even days, and their metabolites keep working. That means your blood sugar can drop overnight, while you’re asleep, or hours after lunch. Glipizide, on the other hand, clears out in a few hours. It’s like turning on a light for a short time - you get the benefit without the lingering danger.Glyburide vs. Glipizide: The Real Difference
Let’s break it down. Glyburide (also called glibenclamide) is the most commonly prescribed sulfonylurea in the U.S. - but it’s also the most dangerous. Data from the FDA’s adverse event system shows glyburide was linked to 68% of all sulfonylurea-related hypoglycemia reports, even though it’s only prescribed about one-third of the time. That’s a red flag. In contrast, glipizide has the lowest hypoglycemia risk among commonly used sulfonylureas. A 2019 study in the American Journal of Managed Care found glipizide caused just 4.2 episodes of serious low blood sugar per 1,000 patient-years. Glyburide? 12.1. That’s nearly three times higher. And it’s not just numbers. Real people are sharing their stories. On the American Diabetes Association’s forum, 72% of users who switched from glyburide to glipizide reported fewer lows. One user wrote: “I was having 2-3 severe lows a month on glyburide. After switching to glipizide, I haven’t had one in six months.” Glimepiride sits in the middle. It’s better than glyburide but not as safe as glipizide. Still, it’s often chosen because it’s once-daily - easier to remember. But if you’re over 65, have kidney problems, or live alone, that convenience isn’t worth the risk.Who Should Avoid Glyburide Completely?
The American Geriatrics Society’s 2023 Beers Criteria doesn’t just caution against glyburide in older adults - it says avoid it entirely. Why? Because as you age, your liver and kidneys don’t clear drugs as well. Glyburide’s active metabolites build up. That means even a small dose can cause hours of low blood sugar - sometimes without warning. A 72-year-old patient on Reddit described spending three days in the hospital after his glyburide dose wasn’t adjusted when his kidney function dropped. His endocrinologist later admitted he shouldn’t have prescribed it. The same applies to people with chronic kidney disease. If your eGFR is below 60, glyburide should be off the table. Glipizide? It’s still safe until your eGFR drops below 30. That’s a big window. And if you’re on insulin or have irregular meals - say, you skip breakfast sometimes or eat late - glipizide’s short action gives you more control. You can take it right before a meal. If you don’t eat? Skip the dose. With glyburide, you’re rolling the dice.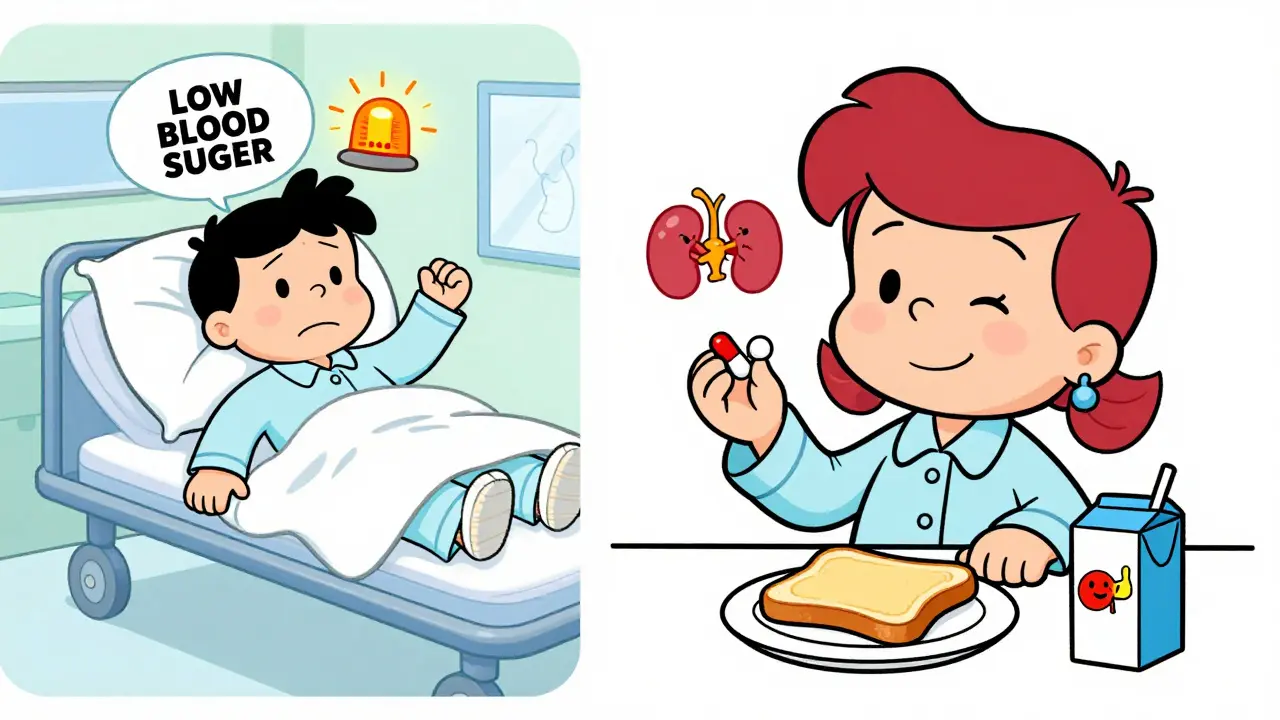
What About Cost? Isn’t Glyburide Cheaper?
Yes, it’s cheaper - but not by much. Glipizide costs about $4.37 a month as a generic. Glyburide? Around $5. Glimepiride? $7. The difference is pennies. But the cost of a hypoglycemic emergency? That’s $1,200 to $5,000 in ER bills, not to mention the stress, missed work, or potential brain injury from prolonged low blood sugar. Newer drugs like semaglutide (Ozempic) cost $500+ a month. But they don’t cause hypoglycemia unless combined with insulin or sulfonylureas. So if you’re choosing between glipizide and a GLP-1 agonist, cost isn’t the only factor. If you’re on a tight budget and need something effective, glipizide is still the safest sulfonylurea.How to Use Sulfonylureas Safely
If you’re prescribed a sulfonylurea, here’s how to stay safe:- Start low, go slow. Glipizide should begin at 2.5 mg, not 5 mg. Glyburide at 1.25 mg, not 2.5 mg. Your body doesn’t need a big dose to work.
- Take it with food. Glipizide works best when taken 30 minutes before a meal. If you skip the meal, skip the dose.
- Know the signs. Sweating, shaking, hunger, dizziness - these aren’t just “bad days.” They’re your body screaming for sugar. Keep glucose tablets or juice on hand.
- Use the 15-15 rule. If your blood sugar drops below 70, take 15 grams of fast-acting carbs (like 4 oz of juice or 3-4 glucose tabs), wait 15 minutes, check again. Repeat if needed.
- Get your kidneys checked. Ask for an eGFR test at least once a year. If it drops below 60, talk to your doctor about switching.
- Don’t take sulfonylureas in the hospital. Your eating schedule changes. Your body is stressed. That’s when hypoglycemia spikes. Hospitals are supposed to reduce your dose by 50% - but many don’t. Ask.



Nicki Aries
I’ve been prescribing glipizide for my elderly patients for years now-especially those with even mild kidney impairment-and I can’t tell you how many ER visits we’ve avoided just by switching them off glyburide. One 81-year-old woman had three hypoglycemic episodes in six weeks on glyburide. Switched her to glipizide 2.5 mg before breakfast, and she hasn’t had a single one in 14 months. She’s back to gardening, traveling, and cooking for her grandkids. This isn’t just pharmacology-it’s dignity.