Eye Infection Treatment Decision Tool
Find the Right Antibiotic for Your Eye Infection
This tool helps you understand which antibiotic eye drop might be best for your specific situation based on severity, history, and other factors. Always consult your doctor for proper diagnosis.
Step 1: Describe your infection
Your Recommendation
Recommended Options
| Medication | Best For | Cost (AUD) | Speed of Relief |
|---|---|---|---|
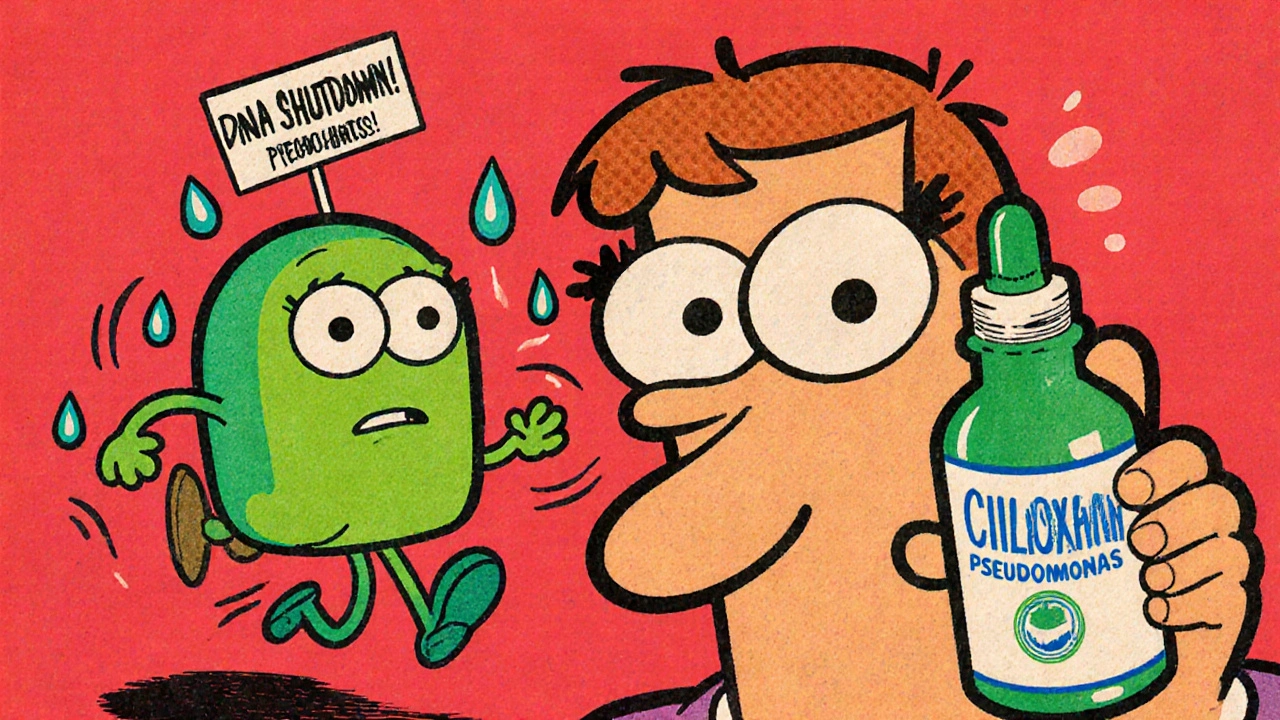
When your eye turns red, feels gritty, or starts leaking pus, you don’t have time to wait. Eye infections move fast. Ciloxan (ciprofloxacin hydrochloride ophthalmic solution) is one of the most common prescriptions doctors hand out for bacterial conjunctivitis, corneal ulcers, and other bacterial eye infections. But it’s not the only option. And not always the best one for your situation.
What Ciloxan Actually Does
Ciloxan is a fluoroquinolone antibiotic eye drop containing ciprofloxacin hydrochloride, approved by the FDA in 1993 for treating bacterial eye infections. Also known as ciprofloxacin ophthalmic solution, it works by stopping bacteria from making DNA, which kills them or stops them from multiplying.
It’s effective against common culprits like Staphylococcus aureus, Pseudomonas aeruginosa, and Streptococcus pneumoniae. That’s why it’s often the first choice for contact lens wearers with corneal ulcers - Pseudomonas loves damp environments like lenses and cases.
Typical use: One to two drops in the affected eye every two hours while awake for the first two days, then every four hours. Treatment usually lasts 7 to 14 days. You’ll often feel relief within 24 to 48 hours - but you still need to finish the full course, even if it feels better.
Why You Might Need an Alternative
Not everyone responds to Ciloxan. Some infections are resistant. Others are caused by fungi or viruses - and antibiotics won’t touch those. Allergic reactions, even rare ones, can happen. And cost? Ciloxan can run over $100 without insurance in the U.S., and even more in Australia where it’s not always subsidized.
Here are the most common alternatives your doctor might suggest - and when each makes sense.
Ofloxacin (Ocuflox)
Ofloxacin is another fluoroquinolone antibiotic eye drop, similar in structure and function to ciprofloxacin. Also known as Ocuflox, it was approved in 1994 and is widely used in Australia and the U.S.
Ofloxacin has a slightly broader spectrum than ciprofloxacin. It works well against gram-positive and gram-negative bacteria, including some strains that have developed mild resistance to Ciloxan. Studies show it’s just as effective for bacterial conjunctivitis and slightly better for certain corneal infections.
Price-wise, generic ofloxacin is often cheaper than Ciloxan. In Australia, it’s listed on the PBS for certain conditions, meaning you pay less out-of-pocket. Dosing is similar: one drop every two hours initially, then tapering off.
Bottom line: If Ciloxan didn’t work after 48 hours, or if you need a more cost-effective option, ofloxacin is a solid next step.
Tobramycin (Tobrex)
Tobramycin is an aminoglycoside antibiotic eye drop, commonly sold under the brand name Tobrex. Unlike fluoroquinolones, it targets bacterial protein synthesis, making it a different class of drug.
It’s especially effective against Pseudomonas aeruginosa - the same bacteria Ciloxan fights, but sometimes more reliably. In hospital settings, tobramycin is often the go-to for severe corneal ulcers, especially when the infection is aggressive or the patient is immunocompromised.
It’s usually dosed every 30 minutes to an hour during the first day, then reduced. That sounds intense, but for serious infections, it’s necessary. Side effects can include mild stinging or blurred vision, but these are usually temporary.
If your doctor suspects a severe bacterial infection - especially if you’ve had trauma, surgery, or wear contacts - they might skip Ciloxan and start with tobramycin right away.

Trimethoprim (Polytrim)
Trimethoprim is a synthetic antibiotic, often combined with polymyxin B in a single eye drop solution called Polytrim. It’s not a fluoroquinolone or aminoglycoside - it blocks folate synthesis in bacteria.
This combo is popular for mild to moderate bacterial conjunctivitis, especially in kids. It’s less potent than Ciloxan or Tobrex but has a very low risk of side effects and is much cheaper. In Australia, Polytrim is widely available over the counter in some pharmacies - though it’s still best used under medical guidance.
It’s not recommended for corneal ulcers or deep infections. But for a red, itchy eye from a common cold or mild contamination, it’s often the first-line choice for GPs.
Chloramphenicol (Chloromycetin)
Chloramphenicol is a broad-spectrum antibiotic that’s been around since the 1940s. It’s available as eye drops under brand names like Chloromycetin. While it’s not used much for systemic infections anymore due to rare but serious blood side effects, it’s still considered safe for topical eye use.
It’s inexpensive, widely available, and effective against many common eye bacteria. In the UK and Australia, it’s often the first antibiotic prescribed for mild conjunctivitis in children and adults - especially when you can’t get a prescription quickly.
Studies show it’s as effective as Ciloxan for uncomplicated bacterial conjunctivitis. But it doesn’t work well for corneal ulcers or infections caused by resistant strains. If your infection is mild and you’re waiting to see a specialist, chloramphenicol can buy you time.
Non-Antibiotic Options: When Antibiotics Aren’t the Answer
Not every red eye is bacterial. Viral conjunctivitis - often from adenovirus - can last up to two weeks and doesn’t respond to any antibiotic. Fungal keratitis, common after plant material injury or contact lens misuse, needs antifungal drops like natamycin.
For viral infections, the treatment is supportive: cold compresses, artificial tears, and time. Steroid eye drops (like prednisolone) are sometimes used alongside antivirals for severe cases, but never alone - they can make viral infections worse.
For allergies, antihistamine eye drops like ketotifen (Zaditor) or olopatadine (Patanol) work better than antibiotics. If your eye is itchy, watery, and swollen - especially if you have seasonal allergies - you’re likely not dealing with an infection at all.
How to Choose the Right One
There’s no single best option. The right choice depends on:
- Severity: Mild redness? Try chloramphenicol or Polytrim. Severe pain, vision loss, or ulcer? Start with tobramycin or Ciloxan.
- History: Contact lens wearer? Prioritize drugs that cover Pseudomonas - Ciloxan or tobramycin.
- Cost and access: In Australia, PBS-listed options like ofloxacin or chloramphenicol are cheaper than Ciloxan.
- Resistance: If you’ve used Ciloxan before and it didn’t work, switch classes - try tobramycin or ofloxacin.
- Age: Kids? Chloramphenicol or Polytrim are often preferred for safety.
Always get a proper diagnosis. Self-treating with leftover drops can delay healing or cause permanent damage.

What to Watch For
Even with the right antibiotic, things can go wrong. Call your doctor if:
- Your vision gets worse after 48 hours
- There’s increased pain, swelling, or sensitivity to light
- You develop a rash or itching around the eye
- The infection returns after finishing the course
These could mean the infection is resistant, fungal, or that you’re having an allergic reaction to the medication itself.
Real-World Comparison: Ciloxan vs Alternatives
| Medication | Class | Best For | Typical Cost (AUD, 2025) | PBS Subsidized? | Speed of Relief |
|---|---|---|---|---|---|
| Ciloxan (ciprofloxacin) | Fluoroquinolone | Corneal ulcers, contact lens infections | $110-$140 | No | 24-48 hours |
| Ofloxacin (Ocuflox) | Fluoroquinolone | General conjunctivitis, resistant strains | $45-$70 | Yes (for certain cases) | 24-48 hours |
| Tobramycin (Tobrex) | Aminoglycoside | Severe Pseudomonas infections | $80-$100 | Yes | 12-24 hours |
| Polytrim (trimethoprim/polymyxin) | Combination | Mild conjunctivitis, children | $30-$50 | Yes | 48-72 hours |
| Chloramphenicol (Chloromycetin) | Broad-spectrum | Mild cases, over-the-counter option | $20-$35 | Yes | 48-72 hours |
Frequently Asked Questions
Is Ciloxan better than ofloxacin for eye infections?
Ciloxan and ofloxacin are very similar - both are fluoroquinolones. Ofloxacin has slightly better coverage against some gram-positive bacteria and is often cheaper and PBS-subsidized in Australia. If Ciloxan didn’t work, ofloxacin is a good next step. But neither is inherently "better" - it depends on the infection type and your history.
Can I use Ciloxan for a viral eye infection?
No. Ciloxan only works against bacteria. Viral conjunctivitis - often caused by cold or flu viruses - will not respond to any antibiotic. Using Ciloxan unnecessarily can lead to resistance and delay proper treatment. If your eye is watery, itchy, and you have a cold, it’s likely viral.
How long does it take for antibiotic eye drops to work?
Most people feel better within 24 to 48 hours. But you must finish the full course - usually 7 to 14 days. Stopping early can let the toughest bacteria survive and come back stronger. If there’s no improvement after 48 hours, see your doctor. You might have a resistant strain or a non-bacterial infection.
Are generic eye drops as good as brand names like Ciloxan?
Yes. Generic ciprofloxacin, ofloxacin, and chloramphenicol contain the same active ingredients and meet the same safety standards. The only differences are in inactive ingredients like preservatives - which rarely affect effectiveness. Most eye specialists in Australia prescribe generics unless there’s a specific reason not to.
Can I buy antibiotic eye drops without a prescription in Australia?
Chloramphenicol and Polytrim are available over the counter in many pharmacies. But even these should be used only for mild symptoms and not for more than 48 hours without seeing a doctor. Ciloxan, tobramycin, and ofloxacin require a prescription. Never use leftover drops from an old infection - they may not be the right drug, and they can be contaminated.
Next Steps
If you’ve been prescribed Ciloxan and it’s not working, don’t switch on your own. Call your doctor. Bring your old drops - they’ll check for contamination or wrong diagnosis.
If you’re trying to save money, ask if a PBS-listed alternative like ofloxacin or chloramphenicol is appropriate. Most GPs and optometrists know the cost differences and will help you choose wisely.
And if your eye still hurts after treatment? Don’t ignore it. A simple red eye can turn into a vision-threatening problem in days. Get it checked - again, if needed. Your eyes don’t heal twice.

joe balak
Just used tobramycin last month for a nasty contact lens infection. Burned like hell for the first hour, but by day two the redness was gone. Ciloxan didn't touch it.