Every time you take an antibiotic when you don’t need it, you’re not just helping yourself-you’re helping bacteria become stronger. That’s the harsh reality behind the rise of antibiotic overuse. What was once a miracle cure is now turning into a global threat. Infections that used to be easy to treat are becoming deadly because the drugs don’t work anymore. And one of the most dangerous side effects? A gut infection called Clostridioides difficile, or C. difficile, that can turn a simple course of antibiotics into a life-threatening ordeal.
Why Antibiotics Are Losing Their Power
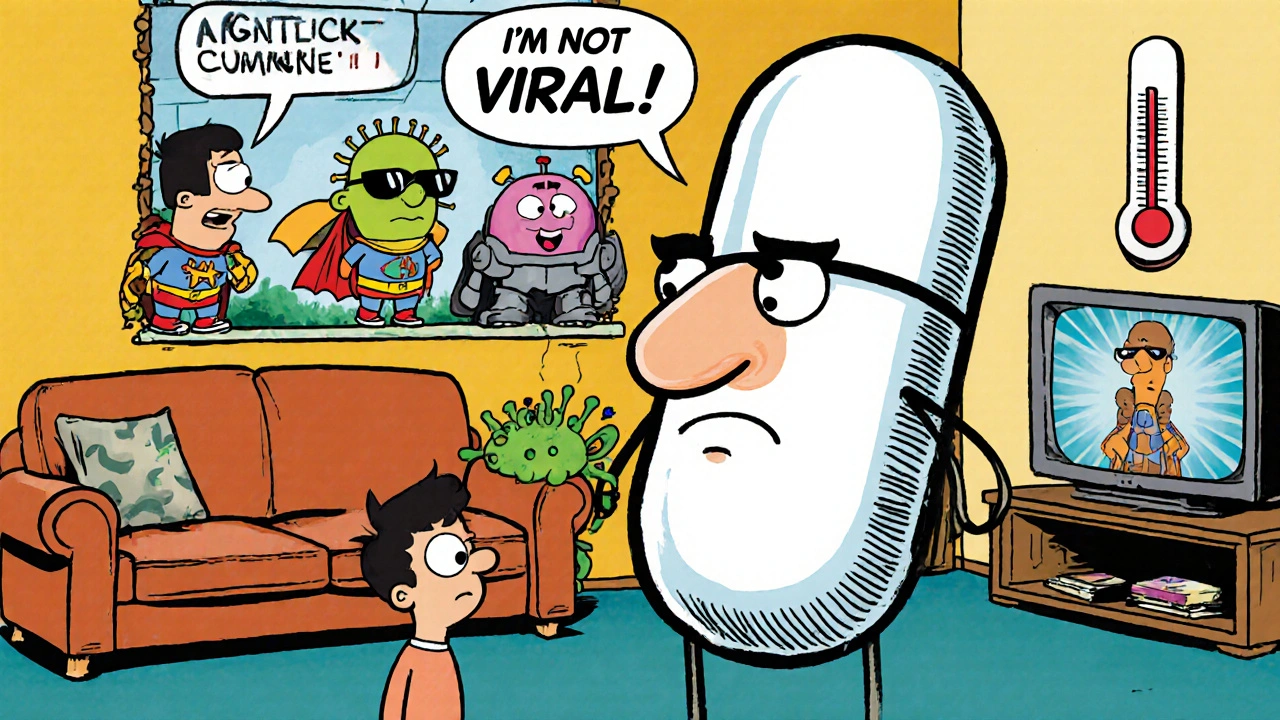
Antibiotics don’t kill viruses. That’s basic. But too often, people ask for them when they have a cold, the flu, or a sore throat-most of which are viral. Doctors, under pressure to satisfy patients or due to lack of quick diagnostic tools, sometimes give in. In hospitals, antibiotics are used as a precaution during surgery or for patients on ventilators. In farms, they’re fed to livestock to make them grow faster or prevent disease in crowded conditions. The result? Bacteria adapt. They evolve. They learn to survive the drugs meant to kill them. This is antibiotic resistance, or antimicrobial resistance (AMR). According to the World Health Organization’s 2025 report, one in six bacterial infections worldwide are now resistant to standard antibiotics. That’s not a future scare-it’s happening right now. Some numbers make it real: 42% of E. coli infections in 76 countries are resistant to third-generation cephalosporins. One in three cases of gonorrhea no longer respond to first-line treatments. Methicillin-resistant Staphylococcus aureus (MRSA) is still common in hospitals and communities. And worst of all, last-resort antibiotics like carbapenems are losing effectiveness. By 2035, resistance to these final options could double compared to 2005 levels. This isn’t just a problem in poor countries. Even in places with advanced healthcare, like Australia, the U.S., or the U.K., resistance is climbing. The WHO says resistance is rising fastest in South Asia and the Eastern Mediterranean-but no country is safe.How Antibiotics Trigger C. difficile
Your gut has trillions of good bacteria. They help digest food, train your immune system, and keep harmful bugs in check. When you take an antibiotic, it doesn’t pick and choose. It wipes out everything-even the helpful ones. That’s when Clostridioides difficile gets its chance. C. difficile is a nasty bacterium that lives quietly in many people’s guts without causing harm. But when antibiotics destroy the balance, it multiplies like crazy. It produces toxins that attack the lining of your colon, causing severe diarrhea, fever, stomach pain, and sometimes life-threatening inflammation. In 2017, the U.S. Centers for Disease Control and Prevention (CDC) reported nearly half a million C. difficile infections. Around 29,000 people died from complications that year. While those exact numbers aren’t confirmed for 2025, trends show the problem is growing. During the COVID-19 pandemic, hospital-based resistant infections jumped by 20%-and C. difficile was one of the biggest contributors. What’s worse? Once you get C. difficile, it’s hard to get rid of. Recurrence rates are high. About one in five people who recover will get it again. And each time it comes back, treatment gets harder. You might need stronger antibiotics, which makes the cycle worse. In some cases, patients need fecal transplants-putting healthy gut bacteria from a donor into their colon-to reset the system.The Silent Pandemic Killing More Than Cancer Could
Antibiotic resistance isn’t just about harder-to-treat infections. It’s about losing the foundation of modern medicine. Think about surgery. Chemotherapy. Hip replacements. C-sections. All of these rely on antibiotics to prevent infections. If antibiotics stop working, these procedures become far riskier. A simple cut could turn into a fatal infection. A broken bone could mean amputation instead of recovery. Experts are warning that by 2050, antimicrobial resistance could cause 10 million deaths a year-more than cancer. That’s not speculation. It’s based on models from Oxford University and Vanderbilt Medical Center. Dr. Kelly Dooley, a leading infectious disease expert, says we’re already seeing cases where doctors have nothing left to offer. No effective drug. No backup plan. Just the helplessness of watching a patient decline. The economic cost is just as scary. By 2030, resistant infections could cost the global economy $3 trillion a year. By 2050, that number could hit $100 trillion. That’s more than the entire global economy in 2020.
Why the Drug Pipeline Is Drying Up
You’d think with this crisis, pharmaceutical companies would be racing to develop new antibiotics. But they’re not. Here’s why: antibiotics are used for short periods. A patient takes them for seven days and gets better. Then they stop. That’s not profitable. Compare that to drugs for diabetes or high blood pressure-people take them for life. Companies make more money selling a pill every day for ten years than they do selling a course of antibiotics. As a result, very few new antibiotics are being developed. Of the 25 antibiotics the WHO says are critically important, many are outdated or in short supply. A 2021 WHO survey found that 64% of countries face shortages of essential antibiotics. Public-private partnerships like CARB-X have invested over $480 million since 2016 to support antibiotic research. They’ve backed 118 projects across 20 countries. But even with that, the pipeline is emptying. We’re running out of time.What Can You Actually Do?
You don’t need to be a doctor or a policymaker to make a difference. Here’s what works:- Don’t demand antibiotics. If your doctor says you have a virus, trust them. Ask what else you can do to feel better-rest, fluids, pain relief.
- Take antibiotics exactly as prescribed. Never skip doses. Never save leftovers for next time. Never share them.
- Ask about testing. If you have a urinary or respiratory infection, ask if a test can confirm it’s bacterial before starting antibiotics.
- Choose meat raised without routine antibiotics. Look for labels like “no antibiotics ever” or “organic.” Your gut bacteria thank you.
- Wash your hands. Simple, but it stops the spread of resistant bacteria in homes and hospitals.
The Bigger Picture: System Change Is Needed
Individual actions matter, but they’re not enough. We need system-wide fixes:- Better diagnostics. Fast, cheap tests to tell if an infection is bacterial or viral-before prescribing antibiotics.
- Antibiotic stewardship programs. Hospitals need teams that review every antibiotic prescription to ensure it’s necessary.
- Global surveillance. Countries must report resistance data honestly and consistently. The WHO’s GLASS system is a start, but coverage is still patchy.
- New economic models. Governments need to pay for antibiotics differently-like they do for vaccines. Pay for results, not volume.
- Regulate farm use. The EU has banned antibiotics for growth promotion. The U.S. is moving slowly. Australia needs to tighten rules too.
What Happens If We Do Nothing?
Imagine a world where:- A child gets a scraped knee, and it turns septic because no antibiotic works.
- A woman needs a C-section, but the hospital can’t prevent infection.
- A cancer patient gets pneumonia, and the only drugs that might help are unavailable.
- A simple tooth extraction leads to a fatal bloodstream infection.
It’s Not Too Late-But Time Is Running Out
We still have time to change course. But not much. The WHO says resistance is rising in over 40% of monitored pathogen-antibiotic combinations since 2018. That’s a fast track to collapse. The answer isn’t just more drugs. It’s smarter use. Better tools. Stronger systems. And ordinary people refusing to accept antibiotics as a quick fix. Every time you say no to an unnecessary antibiotic, you’re not just protecting yourself. You’re helping preserve medicine for everyone else. The next time you or someone you love is prescribed antibiotics, ask: Is this really needed? If the answer isn’t clear, push for more information. Demand better. Because the cost of silence isn’t just money-it’s lives.Can antibiotics cure a cold or the flu?
No. Colds and the flu are caused by viruses, not bacteria. Antibiotics only work against bacterial infections. Taking them for a viral illness doesn’t help you recover faster and only increases your risk of antibiotic resistance and C. difficile infection.
Is C. difficile only a hospital problem?
No. While C. difficile was once mostly seen in hospitals, it’s now common in the community. People who haven’t been hospitalized can get it after taking antibiotics at home, especially older adults or those with weakened immune systems. Community-acquired cases have risen sharply in the last decade.
Are natural remedies like honey or garlic effective against resistant bacteria?
Some natural substances like honey have shown antibacterial properties in lab studies, but they are not replacements for antibiotics in serious infections. Relying on them instead of medical care can delay treatment and make infections worse. They may help with minor wounds or sore throats as supportive care, but never as a substitute for prescribed antibiotics when they’re truly needed.
Why don’t we have more new antibiotics?
Developing new antibiotics is expensive and unprofitable for drug companies. Antibiotics are taken for short periods, unlike drugs for chronic conditions like diabetes or high blood pressure. As a result, pharmaceutical companies focus on more profitable areas. Public funding and new payment models are needed to restart the pipeline.
Can I stop taking antibiotics if I feel better?
No. Stopping early, even if you feel fine, leaves behind the strongest bacteria. These survivors can multiply and cause a relapse-or spread resistance to others. Always finish the full course unless your doctor tells you otherwise.
Are antibiotics in meat really a problem for humans?
Yes. When farm animals are given antibiotics regularly, resistant bacteria grow in their guts. These can spread to humans through undercooked meat, contaminated water, or environmental exposure. Choosing meat labeled "no antibiotics ever" reduces your exposure to these resistant strains.

Karen Willie
It’s easy to feel helpless about this, but I’ve started asking my doctor for tests before accepting antibiotics. Last time I had a sore throat, I asked for a rapid strep test-and they did it. Turned out it was viral. I felt proud of myself for not pushing. Small actions add up.
I also switched to organic chicken after reading this. My gut’s been happier, honestly. Not magic, but worth it.
We don’t need to be perfect. Just more aware.